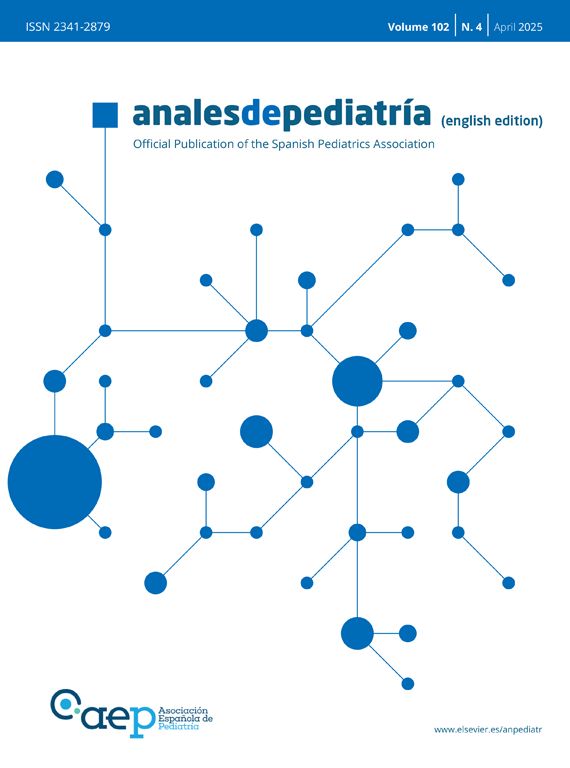
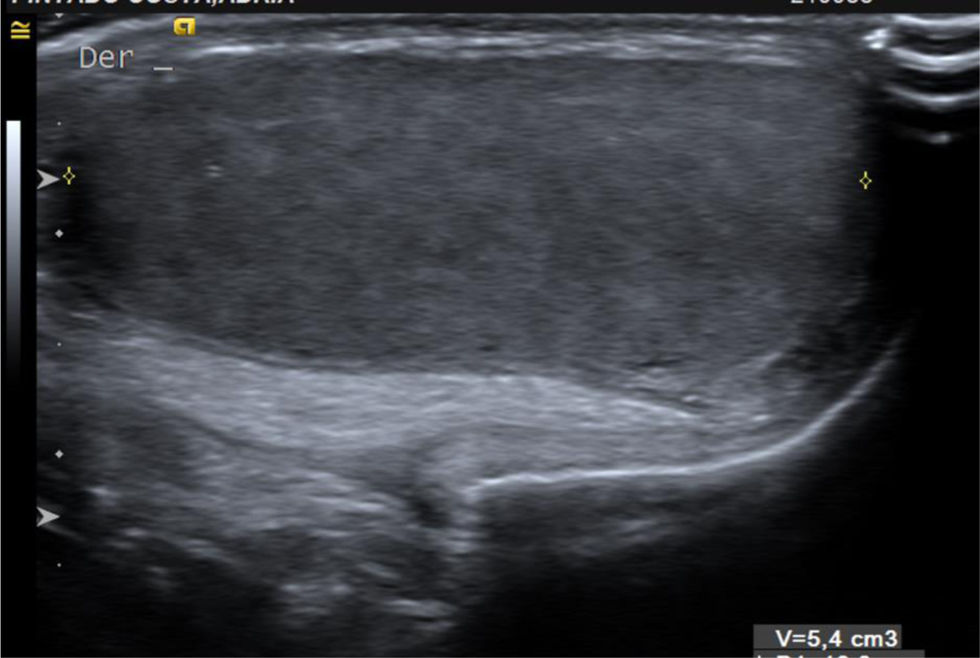
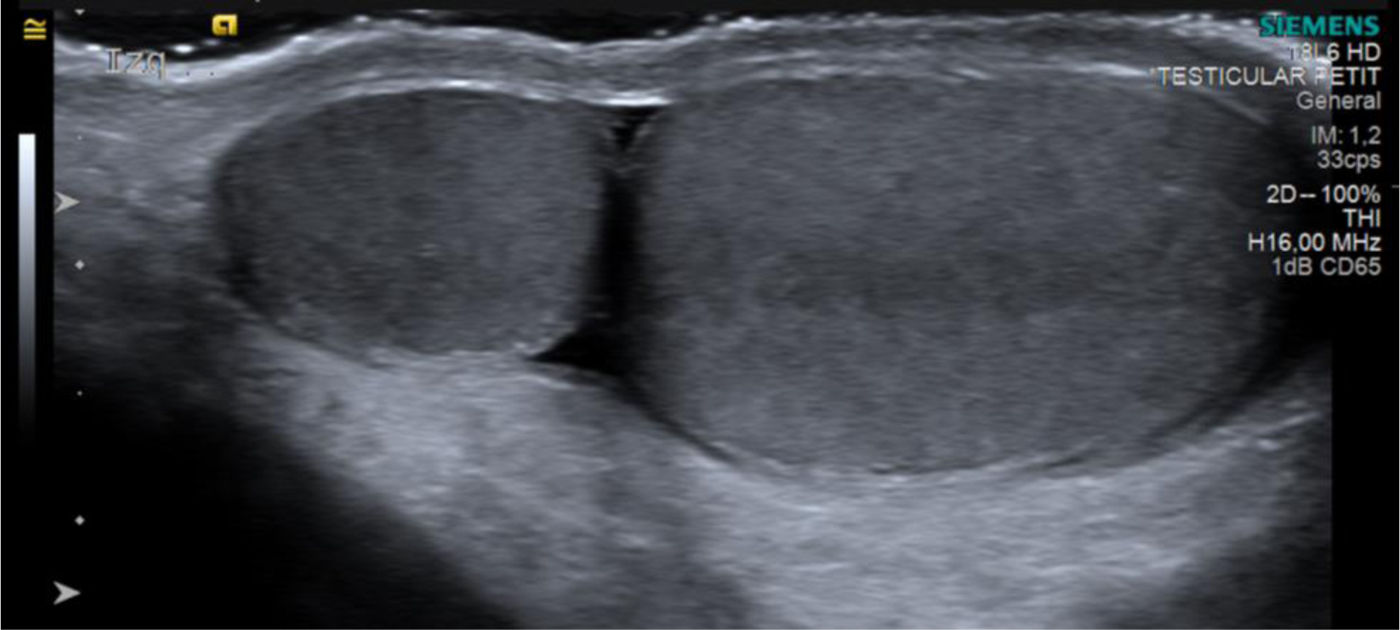
A boy aged 12 years was referred for assessment of testicular asymmetry identified during a routine check-up (left-side volume of 9mL compared to right-side volume of 5mL, measured with an orchidometer). The testicular ultrasound examination revealed a normal right testis (Fig. 1). In the left side, the scan revealed the presence of two ovoid masses with a homogeneous medium-level echotexture, with the mass located cranially measuring 1.3mL and the distal mass measuring 4.8mL (Fig. 2). Both exhibited a hyperechoic area at the center (mediastinum testis) with a thin hyperechoic margin (tunica albuginea) (Fig. 3). The patient received a diagnosis of polyorchidism or left supernumerary testis.
Polyorchidism is a rare condition characterized by the presence of more than two testicles. Triorchidism, defined as the presence of two testicles in one of the scrota, usually the left one, is the most frequent presentation.1
In most cases, the cardinal feature leading to its detection is an asymptomatic scrotal mass. Sonography is the imaging technique of choice, allowing visualization of the supernumerary testis, usually smaller than the contralateral testis, with normal sonographic appearance and preserved blood flow on Doppler.
In some cases, polyorchidism may be associated with inguinal hernia, cryptorchidism, testicular torsion, hydrocele and, more rarely, malignancy.2
The treatment is controversial, with options ranging from a conservative approach with imaging assessments at regular intervals (sonography and/or MRI) to surgical excision on account of the potential for malignant transformation.3