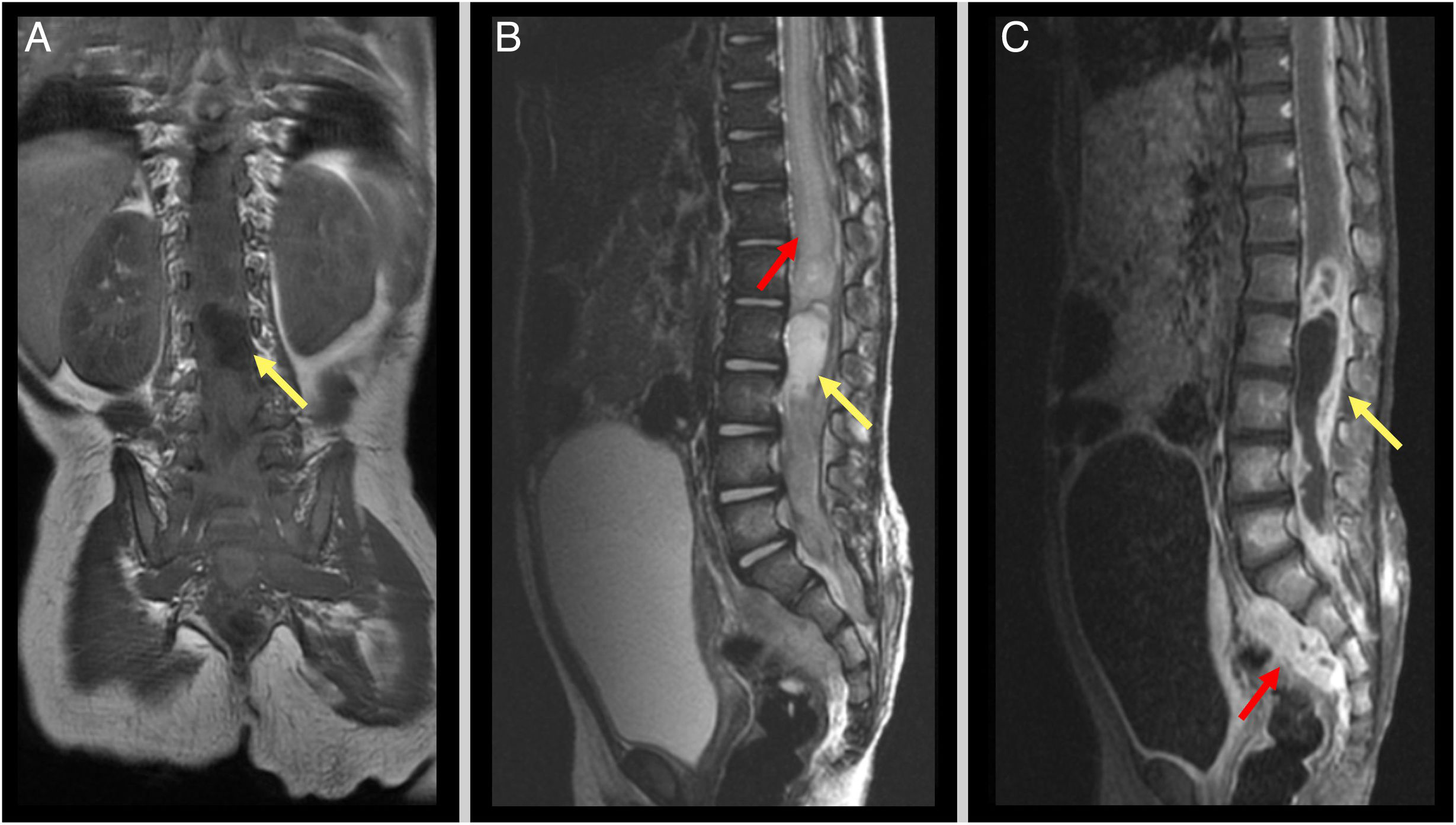
We present the case of a girl aged 2 years brought in for evaluation of lower back dimples and spinal hemangioma diagnosed at birth. She presented with progressive paraparesis with onset 2 months prior, muscle atrophy in the lower extremities, constipation and a tendency to urinary retention and a bulging mass under the hemangioma. The magnetic resonance imaging (MRI) scan showed a large intraspinal mass around the conus medullaris extending into the presacral space with cystic lesions and heterogeneous enhancement (Fig. 1). The complete blood count was normal, with negative results for serum alfa-fetoprotein β-HCG.
Preoperative MRI. (A) T1-weighted image, coronal view: hypointense intraspinal mass (yellow arrow). (B) T2-weighted image, sagittal view, hyperintense intraspinal mass at level of conus medullaris (yellow arrow). Notice the hyperintense signal associated with the large fluid collection in the distal portion of the spine (red arrow). (C) Post-gadolinium T1-weighted image, sagittal view: intradural mass with peripheral tracer uptake immediately below the conus medullaris (yellow arrow) extending to the presacral space (red arrow).
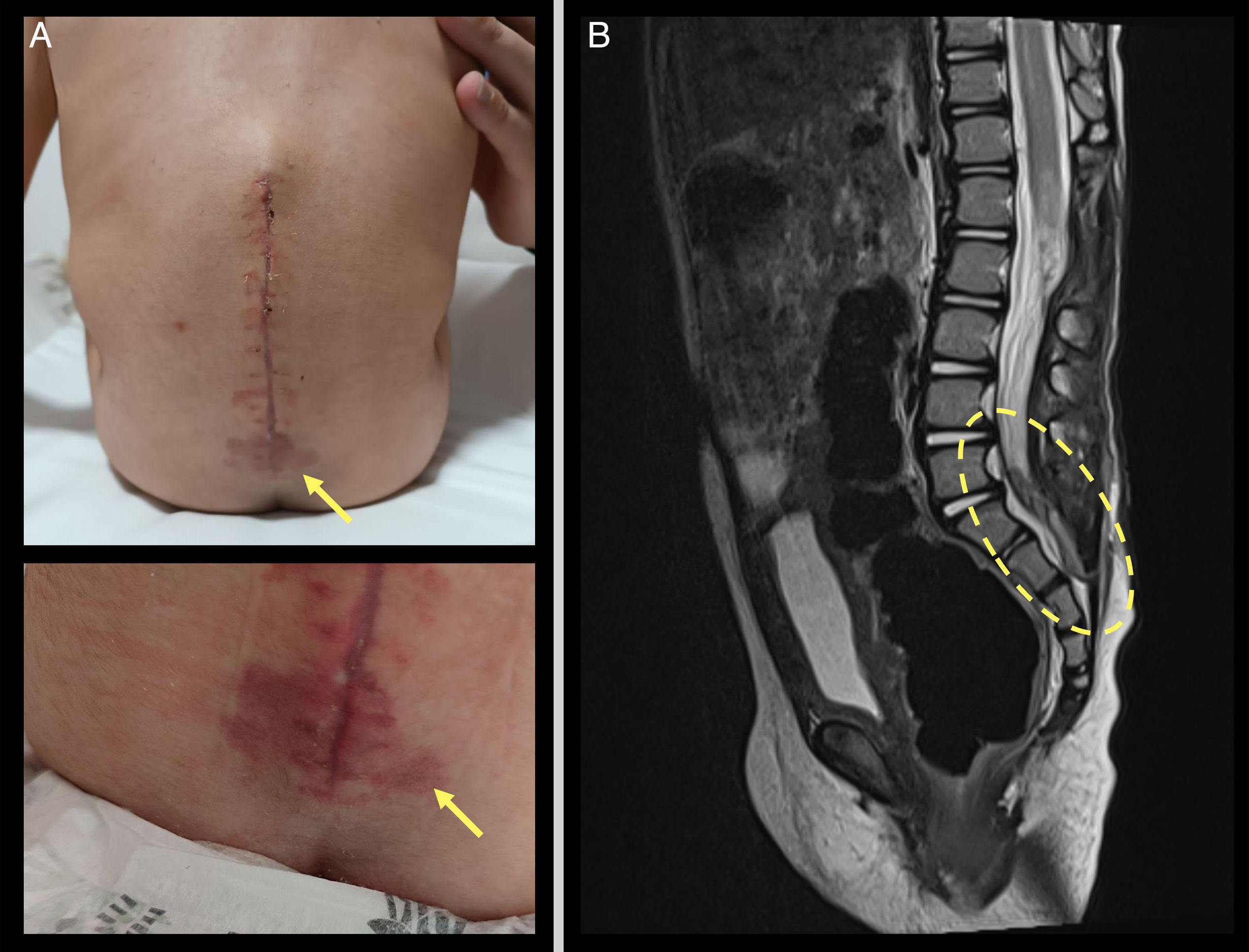
The patient underwent urgent decompression surgery with resection of an encapsulated intradural mass surrounding the conus medullaris with containing purulent material and adnexal masses (Appendix A Video). The histopathological analysis found dermoid cyst superinfection. The patient received a course of broad-spectrum antibiotherapy. During the follow-up, the MRI scan revealed the presence of a previously undetected sacrococcygeal fistulous tract, which was surgically removed to prevent future infections (Fig. 2). At the time of this writing, the sphincter has fully healed, with complete recovery of motor function.
This case illustrates the importance of early identification of the cutaneous stigmata associated with occult spinal dysraphism, as they may be markers of spinal lesions such as dermoid or epidermoid cysts, teratomas or lipomas and which, therefore, should be evaluated upon detection.1 Early characterization can simplify treatment and prevent severe neurologic complications.2,3