Otoscopy is a key method in the diagnosis of acute otitis media (AOM), a very frequent reason for pediatric emergency department (PED) visits. Conventional otoscopy is the most widely used diagnostic technique. However, diagnostic uncertainty and inaccuracy are common in the evaluation of middle ear disease by means of conventional otoscopy, as it may be difficult to visualize the tympanic membrane (TM) in its entirety due to earwax buildup and lack of cooperation in some pediatric patients.1,2 Recent studies have found suboptimal performance in the diagnosis of middle ear disease by both physicians in training and specialists.2,3 In clinical practice, we may find differences in the otoscopic diagnoses of patients initially seen by a medical resident (probably related to their limited clinical experience), which may require repetition of the otoscopic examination, thus increasing the discomfort experienced by the patient. However, digital otoscopy (DO) is a promising alternative, as it offers a more objective interpretation of otoscopic findings, allowing simultaneous visualization of the eardrum by several doctors, and therefore offering an opportunity to enhance medical instruction.4 This prompted us to conduct a study to assess the usefulness of DO performed by first-year pediatrics residents in reducing the need for supervision of otoscopies by the associate pediatrician.
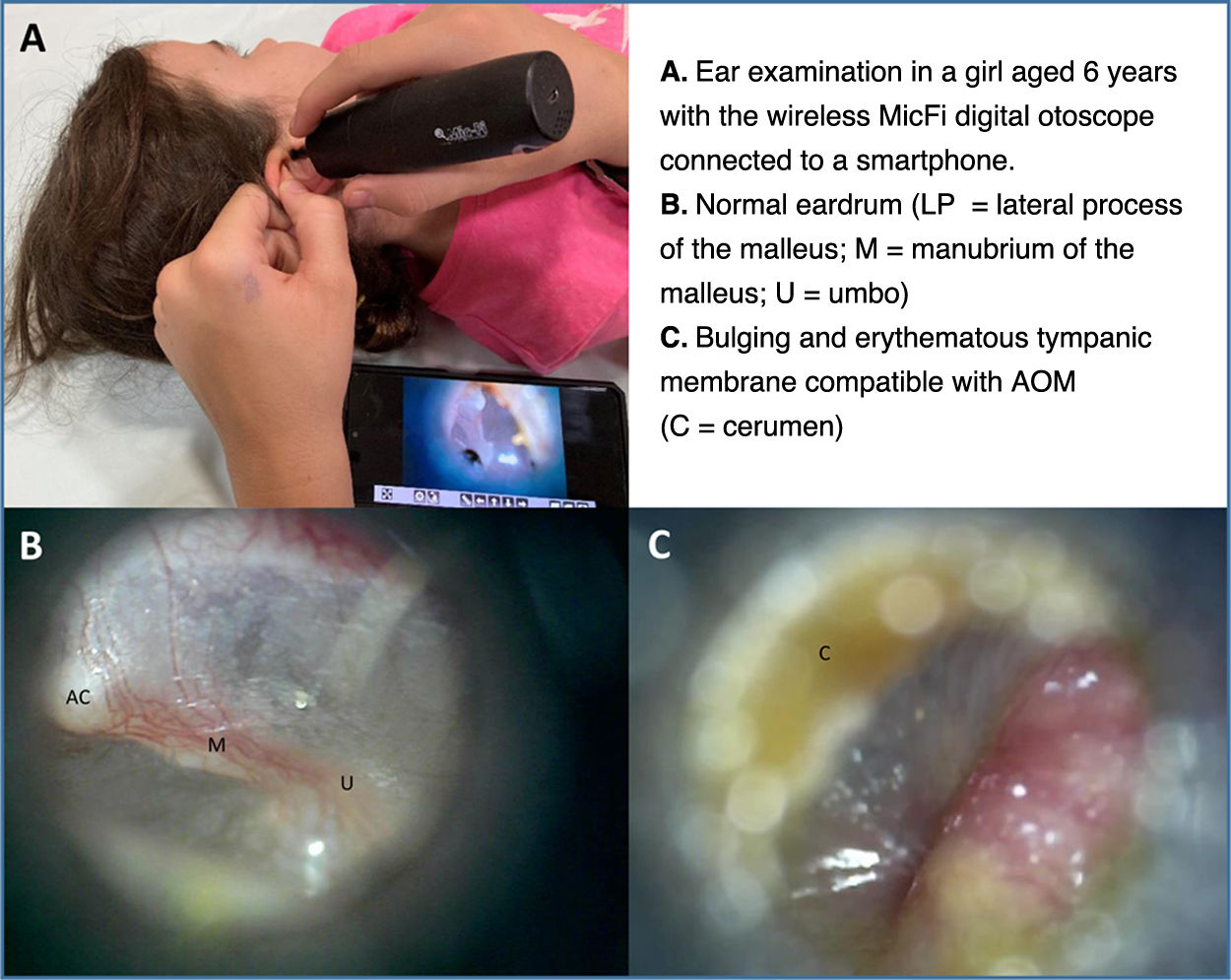
The study was approved by the Clinical Research Ethics Committee of the Hospital Universitario Basurto in Bilbao, Spain. The case series included children presenting with ear pain, nasal congestion and/or fever seen by first-year residents in our PED between November 1 and November 30, 2023. We excluded patients with otorrhea, a history of myringotomy or aged less than 6 months. First-year residents, who had been previously trained in the identification of otoscopic features, performed the initial ear examination with a wireless otoscope (Mic-Fi) connected to a smartphone (Fig. 1). When the resident discussed a patient's case with the attending pediatrician, they showed the videos of the otoscopic examination. The pediatrician then determined whether the second ear examination performed for the purposes of supervision could be avoided. We evaluated two variables, patient age and percentage of the tympanic membrane visualized, and performed a logistic regression analysis to determine which were associated with the decision not to perform the second otoscopy. In addition, the first-year residents completed questionnaires to rate their confidence in performing otoscopies and their satisfaction with the training in pediatric otoscopy training (both rated on 5-point Likert scales).
The study included 172 patients (mean age, 3.6 years [SD, 2.6]; age ≥2 years, 70.3%; male sex, 59.3%) corresponding to 344 ears examined, of which 70.6% (n = 243) did not require a second examination by the attending pediatrician. Of these 243 ears, 55 corresponded to patients aged less than 2 years and 188 to patients aged more than 2 years. In total, there were 157 normal eardrums (45.6%), 71 bulging and/or hyperemic eardrums (20.6%), 27 possible cases of serous otitis media (7.9%) and 89 eardrums that could not be visualized (25.9%). The factors associated with a successful initial examination with DO were: age 2 years or greater (adjusted odds ratio [aOR], 3.1; 95% CI, 1.9–5.2) visualization of more than 50% of the tympanic membrane (aOR, 5.9; 95% CI, 3.5–10.0). In examinations in which first-year residents could visualize the eardrum (74.1% of examined ears), they rated their confidence in interpreting otoscopic findings as “high” (Likert 4/5) or “very high” (5/5) in 79.6% of cases. All first-year residents agreed that DO was “very useful” (5/5) as a teaching tool.
Success in the first attempt with DO may be associated with the possibility of recording the otoscopic examination offered by this technique. In addition, reviewing otoscopy videos and magnifying images makes it possible to identify subtle features,5,6 thereby improving the accuracy of diagnosis, as demonstrated by several studies on the identification of middle ear involvement by physicians,1 which is relevant considering that AOM is a prevalent condition in childhood and that its accurate diagnosis is of the essence.
The possible limitations of this study include the rater-dependent nature of video otoscopy, the absence of a gold standard for diagnosis and the intrinsic limitations of the Mic-Fi otoscope, which, while not offering all the features that would be ideal, proved useful in achieving the intended goal. The reason for excluding infants aged less than 6 months was that the diameter of the smallest available speculum was 3.5 mm, which would have made it difficult to “navigate” the ear canal of the youngest patients without causing them pain.
The use of DO reduces the need to repeat otoscopic examinations in pediatric patients. Thus, it may be a promising alternative diagnostic method. Further studies are needed to explore the potential of DO as a diagnostic and teaching tool.
Previous presentation: this study was presented at the XXVIII Meeting of the Sociedad Española de Urgencias de Pediatría; May 9–11, 2024; A Coruña, Spain.