There is evidence of a worldwide resurgence of syphilis, once nearly eradicated, and the subsequent risk for newborns. The 2022 European annual epidemiological report on congenital syphilis (CS) showed an increasing trend in the number of notified cases after 2020, and Portugal was one of the three countries with the highest incidence in both 2021 and 2022.1 While European data for 2023 are still not available, the Minnesota Department of Health in the United States reported a 44% increase in the regional incidence of CS, with 29 notified cases—the highest in the past 40 years.2 Worldwide, perinatal syphilis is the second leading cause of stillbirth and results in significant of morbidity and mortality.3 Women with untreated early syphilis will pass the infection to 70%–100% of their offspring with the pregnancy ending in stillbirth in 1/3 of cases.3 Vertical transmission occurs late in pregnancy (after 28 weeks), so early treatment of maternal syphilis infection using penicillin prevents fetal complications. In Portugal, pregnant women are screened for syphilis in every trimester with the venereal disease research laboratory (VDRL) test. Screening can also be performed in the delivery room if it was not performed in the third trimester or in the case of high risk or lack of prenatal care.
With the aim of determining the incidence of CS in Portugal, we conducted a retrospective study including children exposed to syphilis in utero and/or with congenital infection in the 2018–2022 period managed in a tertiary care hospital. We collected data on sociodemographic characteristics, maternal VDRL testing and newborn/child titers, coinfections, birth records, maternal treatment during pregnancy, clinical features, treatment of the child and follow-up.
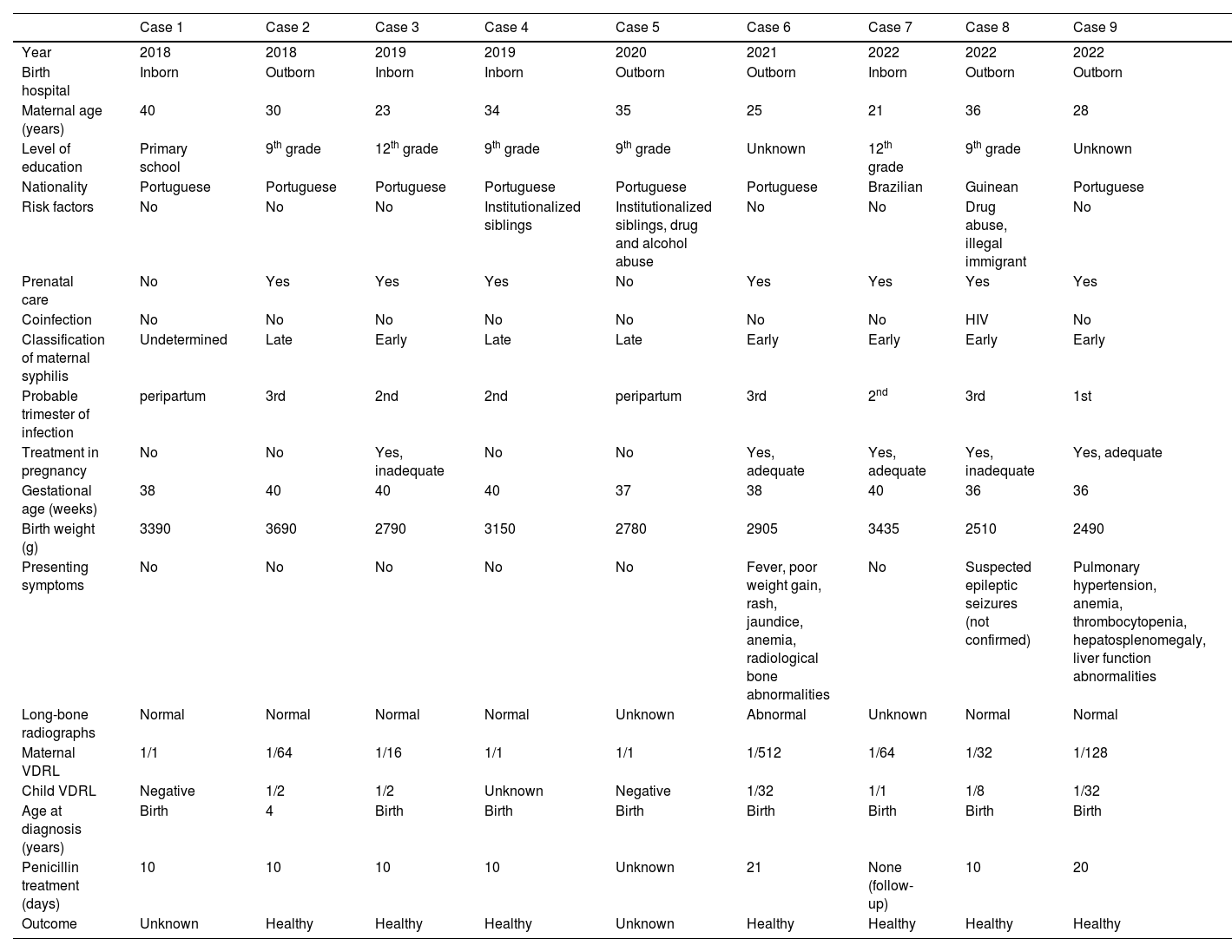
We present the cases of 9 babies born to mothers with syphilis infection. The cumulative incidence for this period was 0.0008% (9/10 731 deliveries), with an annual incidence of 0.0009%, 0.0009%, 0.0005%, 0.0005% and 0.001% from 2018 to 2022. Table 1 summarizes the characteristics of the cohort. All mothers had positive VDRL titers. The maternal characteristics were as follows: 38 % (3) young mothers (age≤25 years), 71% (5) had low educational attainment (elementary education), 57% (4) were unemployed, 22% (2) were from foreign countries (1 Guinean, 1 Brazilian), 11% (1) had coinfection by human immunodeficiency virus, 22% (2) had a history of substance abuse. Three out of seven (43%) mothers who received prenatal care were adequately treated. Maternal syphilis was classified as early in 56% (5), late in 33% (3) and undetermined in 11% (1). Seven newborns had positive VDRL titers. Of these cases, 22% (2) were classified as highly probable CS,4 67% (6) as possible CS4 and 11% (1) as CS less likely.4 There were two cases of early congenital syphilis, one of them manifesting as neurosyphilis. All patients were treated with parenteral penicillin G; 22% (2) were lost to follow-up and the remaining children have been healthy after treatment.
Clinical characteristics of the cases.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Year | 2018 | 2018 | 2019 | 2019 | 2020 | 2021 | 2022 | 2022 | 2022 |
| Birth hospital | Inborn | Outborn | Inborn | Inborn | Outborn | Outborn | Inborn | Outborn | Outborn |
| Maternal age (years) | 40 | 30 | 23 | 34 | 35 | 25 | 21 | 36 | 28 |
| Level of education | Primary school | 9th grade | 12th grade | 9th grade | 9th grade | Unknown | 12th grade | 9th grade | Unknown |
| Nationality | Portuguese | Portuguese | Portuguese | Portuguese | Portuguese | Portuguese | Brazilian | Guinean | Portuguese |
| Risk factors | No | No | No | Institutionalized siblings | Institutionalized siblings, drug and alcohol abuse | No | No | Drug abuse, illegal immigrant | No |
| Prenatal care | No | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Coinfection | No | No | No | No | No | No | No | HIV | No |
| Classification of maternal syphilis | Undetermined | Late | Early | Late | Late | Early | Early | Early | Early |
| Probable trimester of infection | peripartum | 3rd | 2nd | 2nd | peripartum | 3rd | 2nd | 3rd | 1st |
| Treatment in pregnancy | No | No | Yes, inadequate | No | No | Yes, adequate | Yes, adequate | Yes, inadequate | Yes, adequate |
| Gestational age (weeks) | 38 | 40 | 40 | 40 | 37 | 38 | 40 | 36 | 36 |
| Birth weight (g) | 3390 | 3690 | 2790 | 3150 | 2780 | 2905 | 3435 | 2510 | 2490 |
| Presenting symptoms | No | No | No | No | No | Fever, poor weight gain, rash, jaundice, anemia, radiological bone abnormalities | No | Suspected epileptic seizures (not confirmed) | Pulmonary hypertension, anemia, thrombocytopenia, hepatosplenomegaly, liver function abnormalities |
| Long-bone radiographs | Normal | Normal | Normal | Normal | Unknown | Abnormal | Unknown | Normal | Normal |
| Maternal VDRL | 1/1 | 1/64 | 1/16 | 1/1 | 1/1 | 1/512 | 1/64 | 1/32 | 1/128 |
| Child VDRL | Negative | 1/2 | 1/2 | Unknown | Negative | 1/32 | 1/1 | 1/8 | 1/32 |
| Age at diagnosis (years) | Birth | 4 | Birth | Birth | Birth | Birth | Birth | Birth | Birth |
| Penicillin treatment (days) | 10 | 10 | 10 | 10 | Unknown | 21 | None (follow-up) | 10 | 20 |
| Outcome | Unknown | Healthy | Healthy | Healthy | Unknown | Healthy | Healthy | Healthy | Healthy |
Although CS is a preventable disease, it continues to be a major global health problem, and its resurgence reflects deficiencies in prenatal care. Congenital syphilis still has a significant compound impact, and prevention should target specific maternal risk profiles, such as unstable housing, domestic violence, institutionalization, low socioeconomic status, high-risk sexual behavior, substance abuse etc. Shifts in global population demographics and distribution, including rising birth rates among foreign-born mothers in Portugal, could pose challenges to prenatal surveillance, which may affect the incidence of congenital infections. As is known, nearly 90% of syphilis infections occur in low-to-middle income countries (LMICs), with Africa bearing the most critical burden of CS at around 62%.5 Nevertheless, syphilis rates in women of childbearing age have risen by more than 200% in high-income countries with a low incidence of congenital syphilis.6 Further research is required to determine why CS prevention is failing. Applying a unified case definition, reinforcing surveillance, integrating syphilis screening in HIV testing and implementing disease registers could yield crucial data to enhance the management of CS and shape future interventions.6 Thorough screening and treatment (including sexual partners) during antenatal/prenatal care is cost-effective and can decrease the incidence of CS, as evinced by the Chinese plan for the prevention of vertical transmission of syphilis in 2011, which reduced the incidence of CS from 91.6 to 11.9 cases per 100000 live births.7 In addition, we urgently need alternative antibiotics allowing shorter courses of treatment and oral administration to reduce the health care burden.6 Overall, both public health interventions (attracting the attention of the media) and education of health care providers on the matter, namely the early detection of syphilis and its diagnosis and treatment, are warranted to curb this soaring health crisis.
FundingThere was no financial support associated with this paper.
Previous presentation: This work was presented as abstract number 999 at the 41st Annual Meeting of the European Society for Paediatric Infectious Diseases (ESPID).