Peripheral intravenous catheter (PIVC) insertion is one of the most frequent procedures in everyday clinical practice, yet daily care focuses chiefly on central venous catheters (CVCs).1 The use of PIVCs can be complex, with rates of failure before treatment completion of 36% in adults and 25% in children, up to 6% of which cases can be attributed to infection. The overall rate of infection of PVCs may be as high as 1.5%.1,2
The most frequent complications are pain, occlusion, extravasation, phlebitis and dislodgment.2 While PIVC-related infection is not frequent, the use of these devices is so common that these events can add up to significant morbidity associated with substantial increases in costs.1,3
The aim of our study was to analyse the clinical and microbiological characteristics of the complications associated with the use of PIVCs and their impact in terms of antibiotherapy and length of stay.
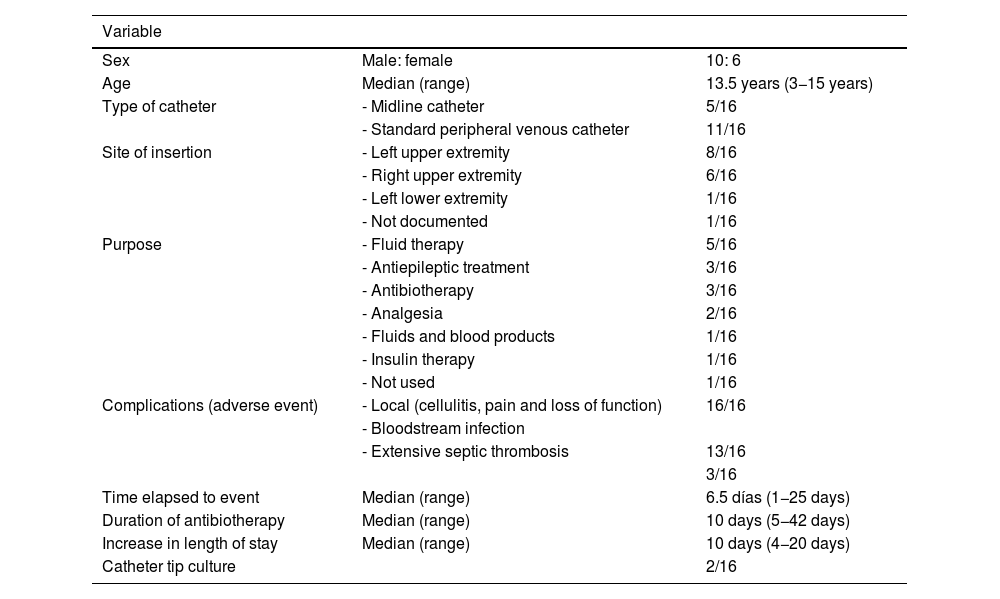
We conducted a retrospective descriptive study through the review of the health records of patients hospitalised in a tertiary care children’s hospital with PIVC-related infection between 2022 and 2023. We analysed variables concerning the demographic characteristics of the patients, the reason for catheterization, complications, microbial isolation and subsequent management. The sample included 16 cases in immunocompetent patients, described in Table 1. None were carriers of a CVC. All patients exhibited local signs of infection (cellulitis and pain with loss of function); in addition, bloodstream infection was diagnosed in 13 patients and septic thrombophlebitis in 3. The median time elapsed from insertion to development of the event was 6.5 days (range, 1−25). All patients receiving fluid therapy and analgesia (7/16) had good oral tolerance. The 13 patients with bloodstream infection received antibiotherapy for a median duration of 10 days (6 weeks if they had thrombosis). In 5 of the 16 patients, complications led to an increase in the length of stay by a median of 10 days (4−20 days). The catheter was removed in every case, but a catheter culture was performed in only two. There were no deaths.
Complications of peripherally inserted catheters.
| Variable | ||
|---|---|---|
| Sex | Male: female | 10: 6 |
| Age | Median (range) | 13.5 years (3−15 years) |
| Type of catheter | - Midline catheter | 5/16 |
| - Standard peripheral venous catheter | 11/16 | |
| Site of insertion | - Left upper extremity | 8/16 |
| - Right upper extremity | 6/16 | |
| - Left lower extremity | 1/16 | |
| - Not documented | 1/16 | |
| Purpose | - Fluid therapy | 5/16 |
| - Antiepileptic treatment | 3/16 | |
| - Antibiotherapy | 3/16 | |
| - Analgesia | 2/16 | |
| - Fluids and blood products | 1/16 | |
| - Insulin therapy | 1/16 | |
| - Not used | 1/16 | |
| Complications (adverse event) | - Local (cellulitis, pain and loss of function) | 16/16 |
| - Bloodstream infection | ||
| - Extensive septic thrombosis | 13/16 | |
| 3/16 | ||
| Time elapsed to event | Median (range) | 6.5 días (1−25 days) |
| Duration of antibiotherapy | Median (range) | 10 days (5−42 days) |
| Increase in length of stay | Median (range) | 10 days (4−20 days) |
| Catheter tip culture | 2/16 | |
The pathogens isolated in blood culture were coagulase-negative staphylococci (5/13), methicillin-sensitive Staphylococcus aureus (3/13), Escherichia coli (2/13), methicillin-resistant S aureus (1/13), Enterobacter cloacae (1/13) and Serratia spp (1/13). Among the 3 cases without bloodstream infection, the following organisms were isolated from the catheter tip: Candida parapsilosis in one and Pseudomonas aeruginosa in another one. In one case, there was no microbial isolation.
Peripherally-inserted intravenous catheter-related infections are health care-associated infections that have not received the attention they deserve, as they increase morbidity and the length of stay after the original reason for admission has been resolved. Our study illustrates the importance of adequate PIVC care in everyday clinical practice given the risk of both local and systemic infection. Although there was a predominance of gram-positive cocci (GPC), consistent with the adult literature, we ought to highlight the 4 cases of bloodstream infection by gram-negative bacilli (GNB), 3 of which resulted in a prolonged length of stay.4 Recent studies in the paediatric population have found greater proportions of infection by GNB compared to GPC and identified frequent contact with the health care system and greater PIVC dwell time as risk factors for GNB involvement.5
The mean PIVC dwell time ranges from 68h6 to 3.9 days3; in our series, the median dwell time was 6.5 days. Thus, the condition of these catheters should be assessed daily by physicians and nursing staff, as well as the need for them (in one case, the catheter was not being used, and in another 6 there were no issues precluding the use of the oral route instead of intravenous access). Our study did not include infants, which constitute the subset of paediatric patients most frequently affected by this complication. This was due to the characteristics of the hospital (which does not provide maternity services and manages patients up to age 18 years) and the high percentage of surgical patients in the sample.
In short, our study evinces the need of a coordinated preventive approach by health care staff to reduce health care-associated infections related to the use of PIVCs in paediatric care settings, reconsidering the indication and need of these devices and optimising aetiological diagnosis by systematically submitting catheter tips to the microbiology laboratory.
It is important that we highlight the limitations of our study, one of which is its retrospective design. In addition, the lack of data on the actual incidence of these events in our hospital is a significant limitation that needs to be addressed in future studies.
Our next step will be a more ambitious prospective study including every patient with a PIVC to be able allowing the assessment of the incidence of complications.
FundingThis research did not receive any external funding.
Declaration of competing interestThe authors have no conflicts of interest to declare.
Previous meeting: this study was presented as an oral communication at the 70th Congress of the Asociación Española de Pediatría; June 6–8, 2024; Cordoba, Spain.