In children, blunt-force inguinoscrotal trauma is infrequent and often dismissed as benign due to its nonspecific presentation, the typically preserved overall condition of the patient, and the absence of overt signs of serious underlying injury. However, certain mechanisms—particularly direct impacts from bicycle handlebars or assaults—may result in significant internal injuries. While most cases initially present with localized pain and swelling, vascular damage,1,2 fascial defects,3 or testicular compromise or dislocation4,5 may go unnoticed without a high index of suspicion. Although the current literature on the subject is limited, several previous case reports describe this type of injury.1–5 Given the scarcity of robust evidence, largely derived from case reports and small series, the true incidence and clinical relevance of these injuries remain unclear. Nevertheless, inguinoscrotal trauma—despite its seemingly benign presentation—is often associated with high-energy mechanisms such as handlebar impacts and therefore warrants careful evaluation. We present a series of five pediatric cases of inguinoscrotal injury due to blunt trauma, underscoring the diagnostic heterogeneity of this condition and the need for systematic assessment in this anatomical region.
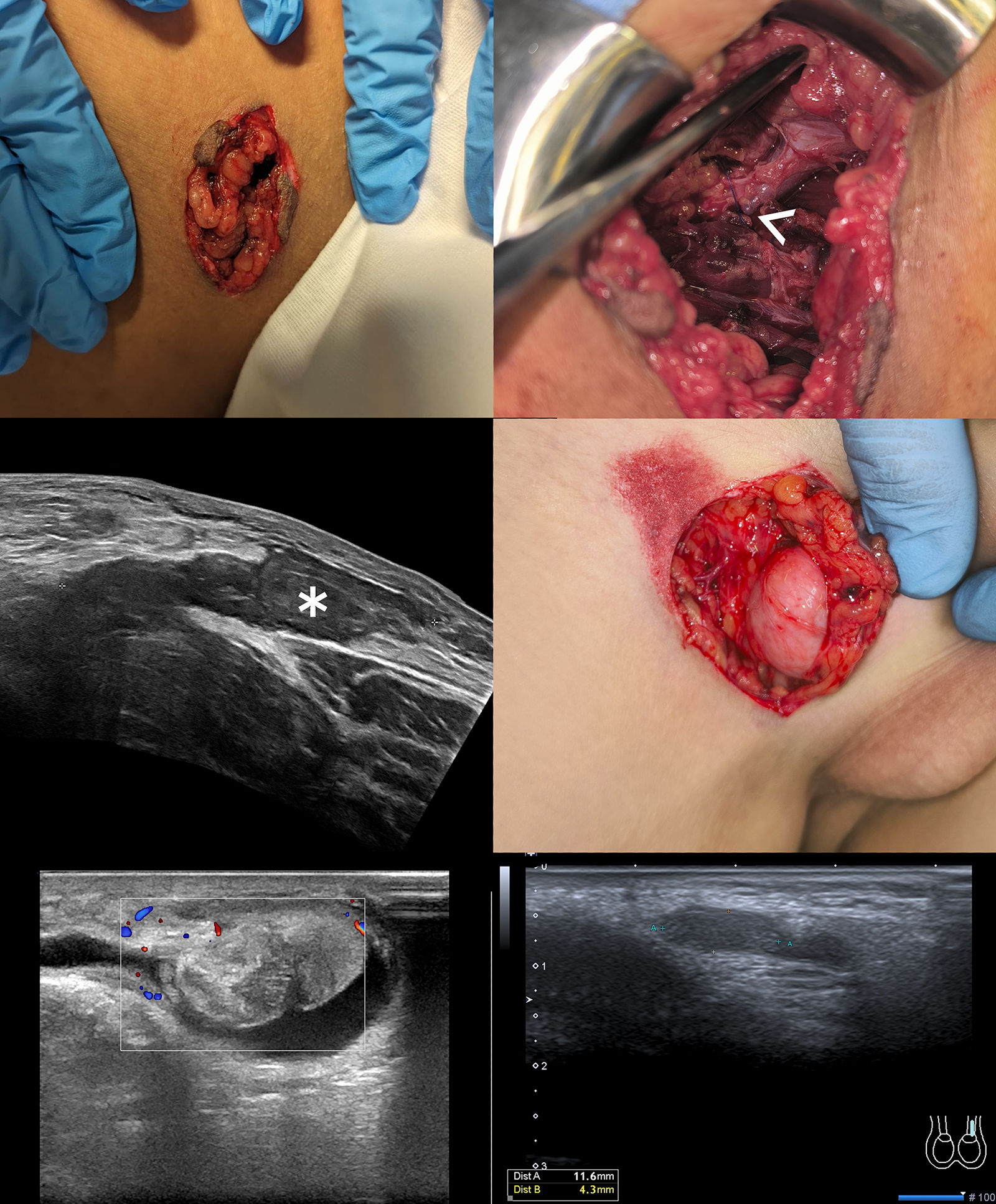
Five male patients were treated for blunt-force inguinoscrotal trauma in our tertiary care pediatric emergency department over a two-year period (Table 1, Fig. 1). The median age (range) was 11 (10-13) years. Four injuries resulted from impact with a bicycle handlebar and one from a direct kick to the scrotum during a physical assault.
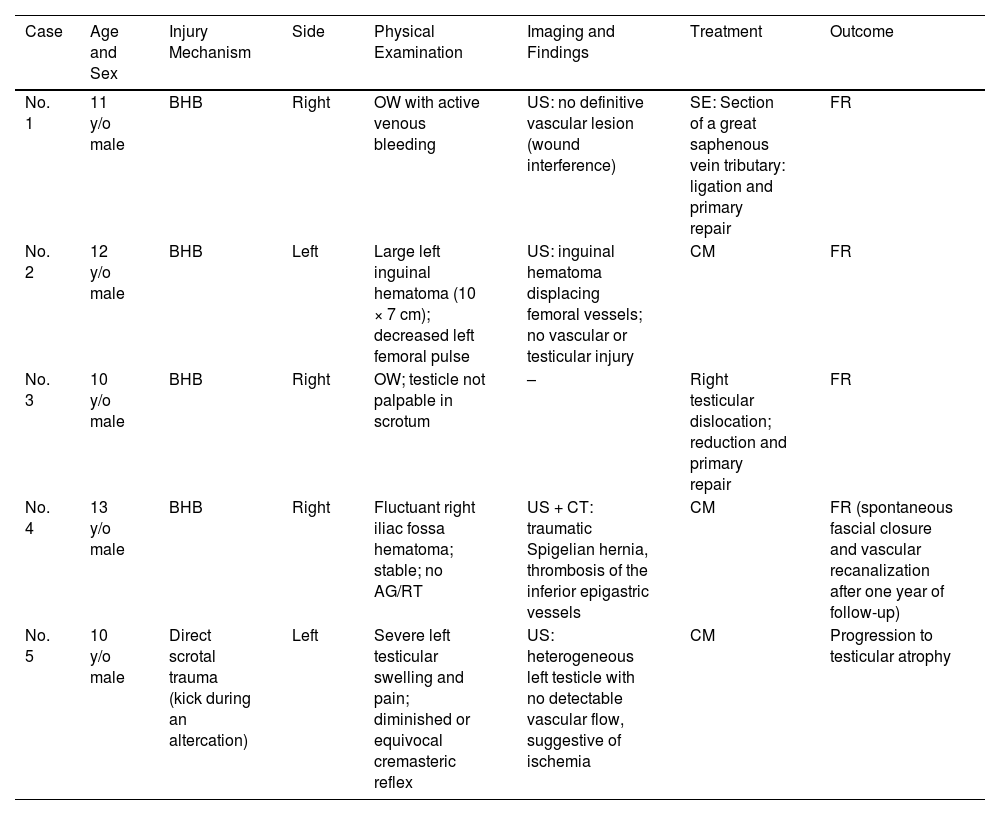
Summary of pediatric inguinoscrotal trauma cases.
| Case | Age and Sex | Injury Mechanism | Side | Physical Examination | Imaging and Findings | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| No. 1 | 11 y/o male | BHB | Right | OW with active venous bleeding | US: no definitive vascular lesion (wound interference) | SE: Section of a great saphenous vein tributary: ligation and primary repair | FR |
| No. 2 | 12 y/o male | BHB | Left | Large left inguinal hematoma (10 × 7 cm); decreased left femoral pulse | US: inguinal hematoma displacing femoral vessels; no vascular or testicular injury | CM | FR |
| No. 3 | 10 y/o male | BHB | Right | OW; testicle not palpable in scrotum | – | Right testicular dislocation; reduction and primary repair | FR |
| No. 4 | 13 y/o male | BHB | Right | Fluctuant right iliac fossa hematoma; stable; no AG/RT | US + CT: traumatic Spigelian hernia, thrombosis of the inferior epigastric vessels | CM | FR (spontaneous fascial closure and vascular recanalization after one year of follow-up) |
| No. 5 | 10 y/o male | Direct scrotal trauma (kick during an altercation) | Left | Severe left testicular swelling and pain; diminished or equivocal cremasteric reflex | US: heterogeneous left testicle with no detectable vascular flow, suggestive of ischemia | CM | Progression to testicular atrophy |
Abbreviations: AG, abdominal guarding; BHB, bicycle handlebar; CM, conservative management; CT, computed tomography; FR, favorable recovery; OW, open wound; RT, rebound tenderness; SE, surgical exploration; US, ultrasound.
Top left: physical examination findings in case No. 1; top right: intraoperative findings in case No. 1. A large-caliber venous structure is observed in the surgical field. Based on its trajectory and topographic relationships, it was presumed to be the great saphenous vein near the saphenofemoral junction. A segmental branch arising from this vessel—already ligated at the time of the photograph—was identified as the bleeding source (white arrowhead); middle left: initial ultrasound of case No. 2, showing an extensive inguinoscrotal hematoma (white asterisk); middle right: physical examination findings of case No. 3, revealing traumatic testicular dislocation; bottom left: initial ultrasound of case No. 5, showing heterogeneous appearance and devascularization of the testis with a small associated hydrocele—findings consistent with severe testicular contusion and vascular compromise; bottom right: follow-up ultrasound of case No. 5 one year after trauma, showing marked testicular atrophy with loss of normal echogenic architecture and reduced dimensions (11.6 × 4.3 mm).
On examination, all five patients presented with localized pain while remaining hemodynamically stable. Two patients presented with open wounds in the inguinal region. Of these two cases, one patient’s wound exploration (case No. 1) revealed brisk venous bleeding (controlled with direct compression), and the other patient (case No. 3) had a traumatic testicular dislocation.
Four patients underwent inguinoscrotal ultrasound (US) as the initial imaging modality. In one of them (case No. 4), abdominopelvic computed tomography (CT) was subsequently performed owing to suspected vascular injury. In one patient (case No. 3), no imaging studies were requested. Radiological findings included a traumatic Spigelian hernia with thrombosis of the inferior epigastric vessels (case No. 4), a heterogeneous left testis with absent vascular flow suggestive of ischemia (case No. 5), and three localized hematomas — inguinal (cases No. 2 and No. 4) or scrotal (case No. 5). In one of the latter (case No. 2), the hematoma caused displacement of the femoral vascular axis, though vessel patency was preserved. In the bleeding patient (case No. 1), a vascular lesion was not conclusively identified on US, probably because the open wound limited optimal transducer placement.
Two patients (cases No. 1 and 3) underwent urgent surgical exploration. In the first one, a severed tributary of the great saphenous vein was identified and managed with ligation and primary layered closure of surrounding soft tissues. In the other patient (case No. 3), the traumatic testicular dislocation was reduced successfully, and disrupted scrotal fascial planes were reapproximated using standard layered closure. The other three patients were managed conservatively.
Clinical outcomes were favorable in four patients. Interestingly, the patient with traumatic Spigelian hernia (case No. 4) exhibited spontaneous clinical and radiological resolution of the hernia, with no residual fascial defect detected on physical examination or follow-up imaging. This finding, although rarely reported in the medical literature, has been previously documented in the context of traumatic Spigelian hernias.6 Additionally, complete recanalization of the inferior epigastric vessels was observed on US. In the assault patient (case No. 5), the condition progressed to complete left testicular atrophy.
Blunt-force inguinoscrotal trauma in children is often underestimated because the external presentation appears benign. However, the present series shows that significant pathology may exist even without alarming signs. Prompt imaging and a high index of suspicion are essential to identify vascular injury, fascial damage, or testicular compromise.
Published reports confirm that bicycle handlebar trauma is a well-recognized mechanism associated with vascular injuries and testicular dislocation. Although most patients with inguinoscrotal swelling have simple hematomas, the possible coexistence of surgically relevant lesions justifies systematic evaluation—especially cases of disproportionate pain, pathological vascular signs, or high-energy mechanisms. Specific clinical signs, such as Brockman’s sign (empty hemiscrotum with a palpable testis in the inguinal or pubic region), may aid early recognition of traumatic testicular dislocation and warrant greater awareness among emergency physicians. In cases of assault-related trauma, thorough documentation and medical and legal reporting are essential due to the clinical and legal implications.
Finally, clinicians should remember that most inguinoscrotal injuries resolve favorably; however, sequelae such as irreversible testicular atrophy can still occur, with long-term implications for endocrine and reproductive health. Prompt identification and close follow-up are key to minimizing these risks.
In conclusion, pediatric inguinoscrotal trauma may involve serious injuries that are not always apparent on the initial gross examination. Emergency clinicians should maintain a low threshold for imaging and surgical consultation, even when initial findings are nonspecific. Critical diagnoses may lie beneath the bruise.