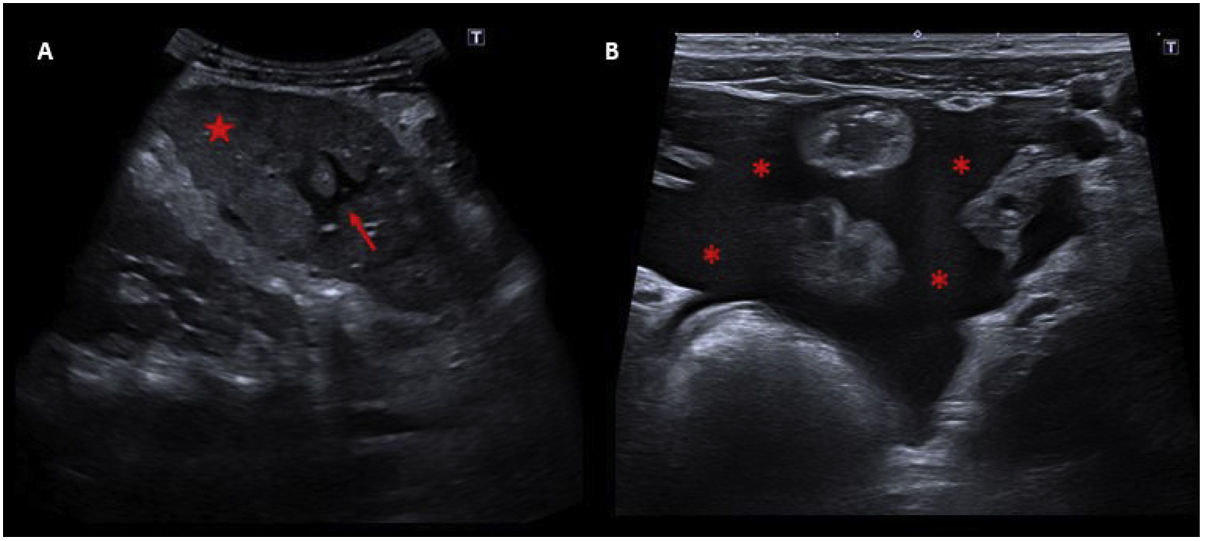
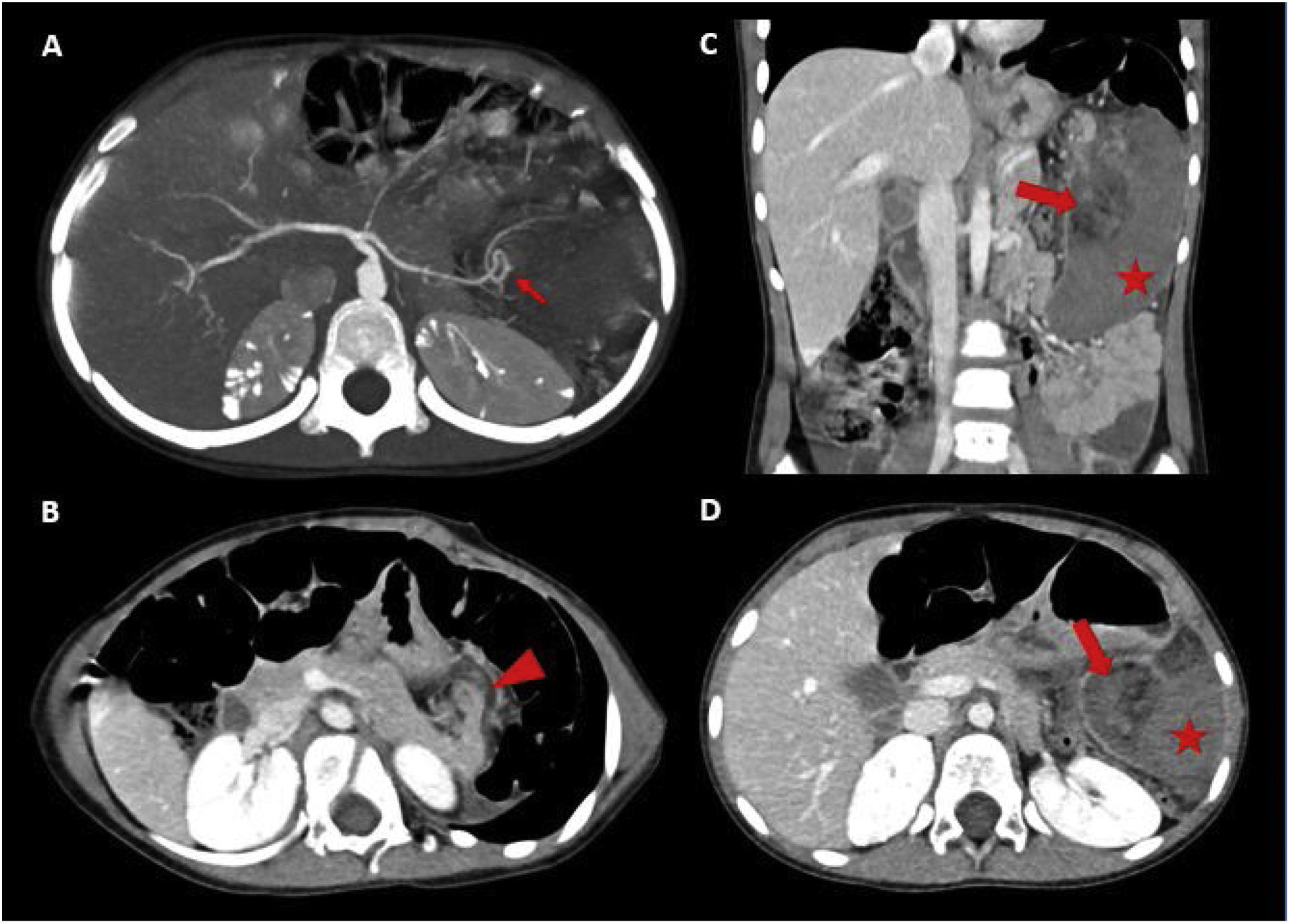
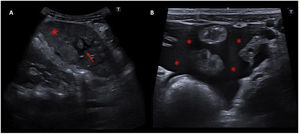
A child aged 4 years presented to the emergency department with abdominal pain of 4 days’ duration without prior trauma. The physical examination revealed the presence of a palpable mass and abdominal guarding in left hypochondrium. Laboratory tests revealed leucocytosis (15.3×109/L), a low haemoglobin concentration (9.5g/dL) and haematocrit (29%), a prolonged prothrombin time (14.7s) and elevation of fibrinogen (888g/L). An abdominal ultrasound scan was ordered, which revealed a moderate amount of intra-abdominal free fluid and an enlarged spleen (13mm) with heterogeneous echogenicity (Fig. 1). An acute process involving the spleen was suspected, prompting performance of a contrast-enhanced abdominopelvic computed tomography (CT) scan that revealed torsion of the spleen along the hilar axis and global splenic infarction (Fig. 2). An exploratory laparoscopy was carried out in the department of paediatric surgery, evincing the absence of splenic suspensory ligaments (SSLs) and with visualization of the previously detected hilar torsion and infarcted spleen, which required splenectomy.
Abdominal ultrasound of the left hypochondrium. A image shows an enlarged spleen (13mm) for the patient's age, with heterogeneous echogenicity (red star). In addition, there were seen geographical areas with well-defined hypoechogenic borders inside the spleen (red arrow), due to ischaemia. B image demonstrates moderate amount of intra-abdominal free fluid (red asterisks).
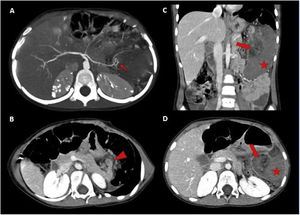
Contrast-enhanced abdominopelvic-CT in arterial phase (A) and portal venous phase (B–D). A image in the arterial phase exposes the splenic artery looping in its final portion at the level of the splenic hilum (red arrow). B image with an anterior displacement of the tail of the pancreas due to torsional traction (red arrowhead). C, D images shows a heterogeneous nodular area fatty content in the splenic hilum compatible with a twisted hilum (red arrow), and an enlarged homogeneously hypodense spleen in relation to massive infarction (red star).
Wandering spleen (WS) is an uncommon entity caused by the laxity or absence of SSLs, resulting in a predisposition to splenic torsion with rare involvement of other organs.1,2 It is usually found in children aged less than 10 years,1,3 and its clinical presentation ranges from the presence of an asymptomatic abdominal mass to acute abdomen due to splenic infarction.3 Sonography is the main imaging test used for diagnosis of WS, but contrast-enhanced CT or magnetic resonance imaging contributes information on the viability of the spleen that is key to decide whether splenectomy is required.1,3