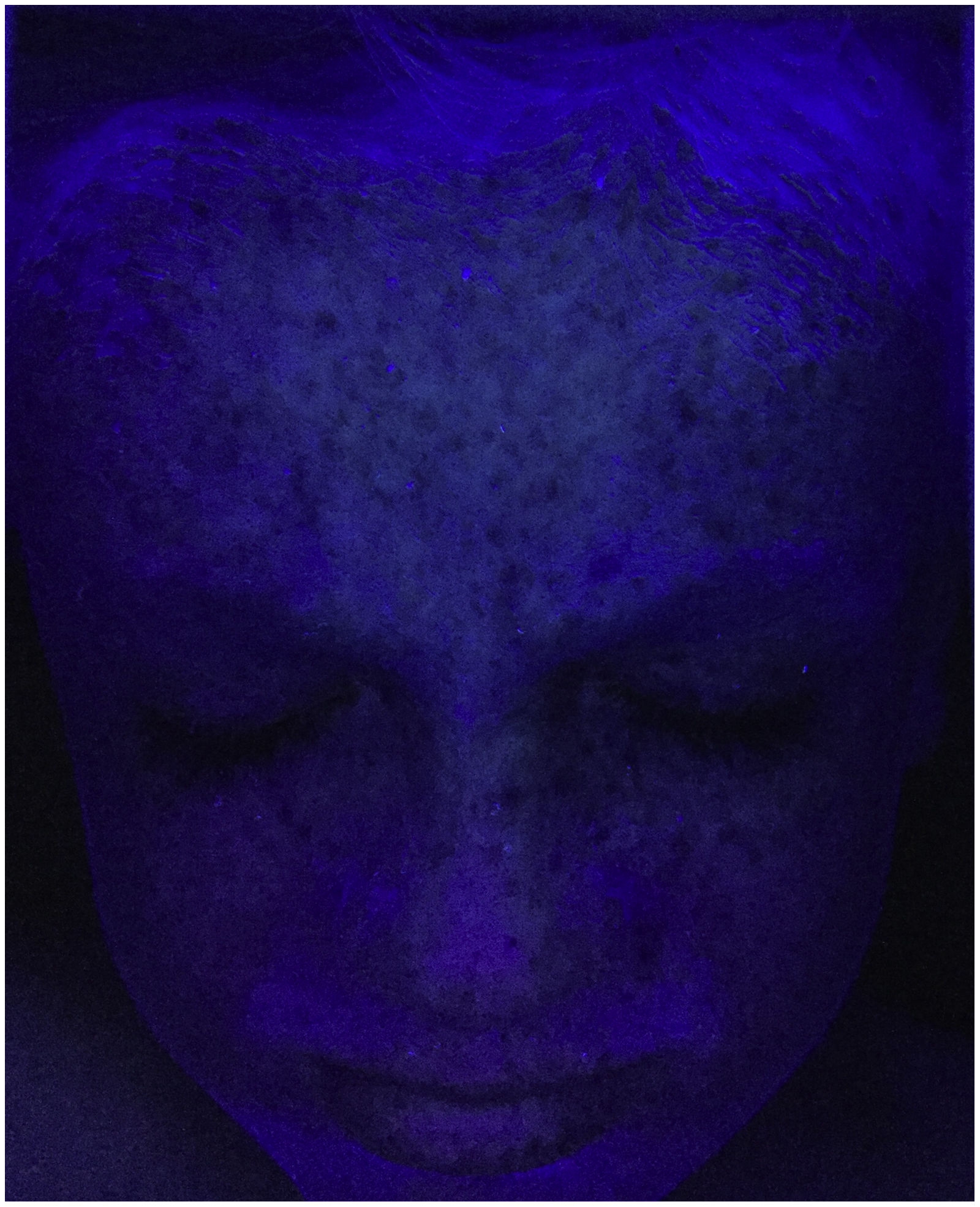
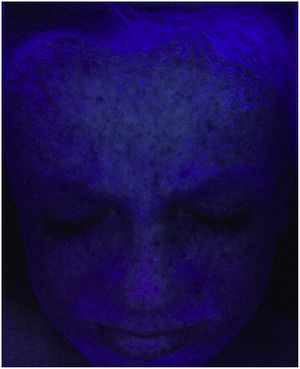
We present the case of a boy aged 20 months, of European ancestry, born to consanguineous parents (second cousins). From 1 year post birth, he developed multiple ephelides clustered in areas exposed to sunlight, chiefly in the face (Figs. 1 and 2), leading to the clinical diagnosis of xeroderma pigmentosum (XP). The diagnosis was confirmed with the detection of the homozygous pathogenic variant c.1643_1644delTG (p.Val548Alafs*25) in the XPC gene, associated with XP type C. Both parents, who were asymptomatic, carried the variant in a single allele. There was no evidence of ophthalmological or neurologic involvement. The examination of the hair with polarised light microscopy did not reveal abnormalities.
Xeroderma pigmentosum XP is a rare hereditary skin disease (prevalence, 1–2.3/1 000 000) characterised by extreme cellular sensitivity to ultraviolet radiation associated with changes in genes involved in DNA repair.1 It has an autosomal recessive pattern of inheritance, and there are 8 subtypes: XP type A through G and XP variant.2,3 It manifests with multiple ephelides from age 1–2 years in areas exposed to sunlight, sunburn after short exposures, premature skin ageing, increased risk of skin cancer (squamous cell/basal cell carcinoma, melanoma) and ophthalmological and neurologic abnormalities.1–3 The latter are infrequent in XP group C, which is most common in Spain.2 It can be diagnosed based on clinical features and confirmed with molecular methods.3 The goal of management, based on lifelong avoidance of exposure to ultraviolet radiation, is the prevention and early detection of skin cancer from a young age.1,3