Asthma, the most prevalent chronic disease in pediatric age, continues to pose challenges in its management and treatment. National and international guidelines emphasize the importance of therapeutic education (TE) to achieve disease control. TE involves imparting knowledge and skills to the patient and their family, enhancing medication adherence, rectifying errors in inhalation technique, and tailoring treatment based on individual patient characteristics.
It is essential for TE to be progressive, gradual, and personalized, spanning all levels of care. Training healthcare professionals in TE is crucial, particularly for pediatricians, who must also be aware of the extensive variability of available meds and inhalers and their respective age-specific indications.
Addressing this need, the REGAP Group extensively reviewed inhalers currently available in Spain for pediatric asthma treatment. The review encompassed different inhalation systems and inhaled drugs used for pediatric asthma treatment. This review will be updated annually, providing information on medications, devices, inhalation chambers, indications, and financiation. The REGAP Group hopes that these tables will be a valuable help for pediatricians in their daily clinical practice and serve as an effective TE tool.
El asma, la enfermedad crónica más prevalente en la edad pediátrica, continúa planteando desafíos en su manejo y tratamiento.1 Guías nacionales e internacionales destacan la importancia de la educación terapéutica (ET) para lograr el control de esta enfermedad.2,3 Esta educación implica la transmisión de conocimientos y habilidades al paciente y su familia, mejorando la adherencia a la medicación, corrigiendo errores en la técnica de inhalación y ajustando el tratamiento según las características individuales de cada paciente.4,5
Es esencial que la ET sea progresiva, gradual e individualizada, y que esté presente en todos los niveles asistenciales. La formación en ET de profesionales sanitarios es crucial, especialmente para los pediatras, quienes además deben conocer la extensa variabilidad de medicamentos e inhaladores disponibles y sus indicaciones para cada edad.6
Para abordar esta necesidad, el Grupo REGAP ha revisado exhaustivamente los inhaladores actualmente disponibles en España para el tratamiento del asma en la edad pediátrica. La revisión incluye una revisión de los distintos sistemas de inhalación y los distintos fármacos inhalados, utilizados para el tratamiento del asma en la edad pediátrica. Esta revisión se actualizará anualmente, incluyendo información sobre fármacos, dispositivos, cámaras de inhalación, indicaciones y financiación. El Grupo REGAP espera que estas tablas sean una valiosa ayuda para los pediatras en su práctica clínica diaria y constituyen una eficaz herramienta de ET.
The Spanish Network of Working Groups on Paediatric Asthma (known as REGAP) gathers all paediatric scientific societies related to asthma. It was created with the purpose of reviewing various topics related to asthma in children and adolescents to facilitate the work of the different health care professionals that serve paediatric patients with this condition. In 2021, the REGAP published a consensus document on the diagnosis and treatment of paediatric asthma,7 and, in the present document, the aim of the REGAP is to provide an update on the different drugs and inhaler devices used most frequently in the management of paediatric asthma currently available in Spain.
Asthma is the most common chronic disease of childhood and has a substantial impact at the personal, family, economic and social levels. It affects approximately 10% of the paediatric population and its prevalence continues to grow.7,8 The goal of asthma treatment is for patients to achieve the greatest possible degree of control over the disease, with establishment of individualised, adapted and specific goals for each patient and family. The number of asthma drugs continues to grow, as does that of the devices adapted to the needs of different patients. treatment of asthma. Despite all these advances, the prevalence of poorly controlled asthma continues to be excessively high, giving rise to a high demand for health care services, both at the primary care and hospital levels. The promotion of adherence to maintenance medication and the assessment of inhaler technique are two key elements of asthma education (AE) to achieve control of the disease, and, in order to deliver quality AE to patients with asthma and their families, it is essential for all professionals managing childhood asthma to be aware of the various treatment options that are currently available.8,9
At present, a large variety of inhaler devices and inhaled drugs are available for the management of childhood asthma in Spain. The inhaler devices funded by the public health system vary among the autonomous communities, and the indications and recommendations for their use by age group are updated and modified on an ongoing basis, so it may be challenging to keep abreast of the latest changes. For this reason, the REGAP decided to make an up-to-date review of the inhaled medications and inhaler systems and devices most widely used for treatment of asthma that are currently available in Spain.
The aim of this document was not to provide an exhaustive review of every available treatment option nor a guideline for the management of asthma, but to offer an up-to-date, simple, practical and general overview with graphic summaries offering essential information of the drugs and devices used most frequently in inhaled therapy for asthma in the paediatric population. This review will be updated annually and made available through the websites of the different scientific societies that compose the REGAP with the main objective of helping health care professionals stay updated about the different treatment options.
We want to take this opportunity to restate the need to ensure equal and universal access to inhaled asthma medications in Spain and underscore that the RECAP considers that every paediatric patient should have publicly funded access to an age-appropriate spacer and also facemasks if needed. We consider the establishment of public funding of spacers and facemasks in every autonomous community in Spain an urgent need.
Our aim is for this review to be a very helpful resource for all health care professionals involved in the management of asthma patients and their families.
Asthma in the paediatric populationAsthma is a heterogeneous disease characterised by a series of clinical manifestations reflecting the presence of chronic and reversible obstruction of the lower airway.2,3,7 According to the World Health Organization (WHO), it affects more than 7 000 000 children worldwide, causes significant mortality and constitutes an important economic burden.10,11 Studies in Spain show that asthma is the most frequent chronic disease in the paediatric population, with a prevalence of approximately 10% and an increasing trend in its incidence.12–14 This trend elicits crucial questions about the causes of this increase and evinces the pressing need to develop more effective prevention, diagnosis and treatment strategies.15–17
The correct diagnosis of asthma is mainly based on a detailed physical examination and history-taking and, when possible, lung function tests, including performance of spirometry and a bronchodilator reversibility test. Asthma has 4 cardinal or main symptoms: cough, dyspnoea, wheezing and chest tightness.3 Identifying and assessing the severity of disease is essential for the purpose of developing a personalised treatment plan. The management of asthma combines preventive measures, control of triggers, use of appropriate medication and AE.7 The objective is not only to reduce the frequency of acute asthma exacerbations, but to achieve a good quality of life, maintain adequate pulmonary function, achieve the greatest possible control of the disease and minimise comorbidities and adverse events in the short and long term.
The importance of health education in asthmaDomestic and international guidelines underscore the importance of AE to achieve control of this disease.2,3 Asthma education entails the transmission of knowledge and skills to the patient and the family to improve adherence to medication, correct errors in inhaler technique and adjust the treatment based on the individual characteristics of each patient.4,5 This education must be personalised and delivered gradually and progressively at every level of care. Along with the prescribing and consumption of inhaled medication, AE is one of the cornerstones of the effective management of asthma. Strict adherence to medication and correct inhaler technique are crucial elements in ensuring optimal asthma control.18 Patients that fully understand their condition and treatment are better prepared to make informed decisions about their health and keep the symptoms of asthma under control.19–22 A structured education plan must include an outline detailing the knowledge and skills that the patient needs to learn and a methodological guideline describing how providers should deliver this education.23
In this regard, it is of the essence that health care professionals, and paediatricians in particular, have the necessary skills to provide effective AE. Paediatricians play an essential role in guiding young patients and families in the daily management of asthma.24 Providers need to be acquainted with the different inhalers available and their correct use in order to train patients and families effectively in the acquisition of these skills. Thus, the REGAP undertook the development this review so that it could be used as an aid in AE, offering a visual and simple summary of the treatments currently available for paediatric asthma, thereby facilitating the day-to-day work of health care professionals.
Available drugs and inhaler systemsAsthma medication is quite varied, with a broad range of commercially available drugs and inhaler devices and new drugs or indications being introduced on an ongoing basis. Inhaled medications vary in terms of composition, dose, dosage forms and, what is more important, indications. This variety can be overwhelming for both paediatricians and other health care professionals involved in the care of children with asthma. Previous studies have found a low level of knowledge on this aspect in health care professionals.25–28
Inhaled bronchodilators and systemic corticosteroids are the mainstay of the management of asthma exacerbations.
- -
Short-acting β2 adrenergic agonists (SABAs) or short-acting bronchodilators are the main treatment for asthma exacerbations. The most widely used SABA is salbutamol, which should be administered, preferably, with a pressurised inhaler and a spacer, as this is as effective as administration with a nebulizer, has fewer side effects and is more cost-efficient, even in severe exacerbations. Administration with a nebulizer can be considered in severe exacerbations or special situations, in which case high oxygen flow rates should be used (8L/minute) to achieve small particles that can spread throughout the entire bronchial tree. The oral route is not considered appropriate for SABA. It is possible to use other inhaled bronchodilators for management of exacerbations, such as terbutaline (another SABA) or ipratropium bromide (a short-acting anticholinergic). All patients with asthma, independently of their age and the type of device they usually employ, should have a pressurised inhaler for administration of salbutamol through a spacer for symptom management during acute exacerbations.
- -
Systemic corticosteroids are administered through the oral route (first-line treatment), reserving the parenteral route for patients who cannot tolerate oral administration or with severe exacerbations.
The goals of pharmacological maintenance therapy for asthma are to reduce the inflammation of the airway, control symptoms and minimise future risks, such as exacerbations and decreased pulmonary function. Maintenance therapy must be individualised and continuously adjusted based on the aetiological and pathophysiological factors, the severity of disease and the response to treatment to achieve the greatest possible degree of disease control and reduce the risk of adverse events, economic costs and the efforts that these measures require along with their impact on the life of the patient and the family.
With a few exceptions, pressurized inhaled medication must always be administered with a spacer, also known as a holding chamber. This spacer be used with a face mask in young children. The face mask is essential in infants, very young children or non-cooperating children, but its use entails an increased dead space so it should be removed once it is ascertained that the child can correctly inhale through the mouthpiece of the spacer.28 This is usually achieved by age 4–6 years, but it depends on the skill, ability and inhaler technique of each child.
It is essential that providers be acquainted with the different types of inhalers and the technique for their use. Inhaler technique should be taught broken down in steps, demonstrating it in the clinic and verifying that the patient can use the inhaler correctly before prescribing this type of medication.
We ought to mention that, broadly speaking, 2 types of devices are currently available to deliver inhaled medication: pressurised MDIs and dry powder inhalers.
Metered-dose inhalers and spacersMetered-dose inhalers (MDIs), also known as pressurised inhalers or “puffers”, are characterised by delivering a fixed dose of the drug with each puff. The medication is contained in a metal canister, where the active ingredient, generally in the solid phase, is suspended in a liquid propellant. The canister is housed in a case that holds the metering valve that allows the delivery of a fixed dose of the drug. Since the drug is a suspension, the device must be shaken prior to its administration to ensure delivery of a fixed dose with a homogeneous concentration of the drug. Most asthma drugs are available in this type of inhaler. Some MDIs have dose counters that let the user know how many doses have been delivered and how many are left, information that is very useful for the patient and the prescribing physician. In devices that do not have a counter, it is possible to estimate the remaining amount of medication by placing the metal canister in a container filled with water; if the canister is empty it floats to the top, it if still has a large amount of medication it is heavy and sinks to the bottom, and if it is approximately half-full it will be floating about the middle of the container. Inhalers with counters are unquestionably a simpler, safer and more effective way to calculate the remaining amount of medication.
All pressurized MDIs should be used with a spacer, a recommendation supported by the different asthma management guidelines. The use of a spacer reduces the oropharyngeal effects of the drug, does not require that the child coordinate the puffing of the device with the intake of breath, and makes it possible for the ejected particles to reach the furthest recesses of the airway. In very young or non-cooperating children, face masks should be used, preferably clear, flexible and tight-fitting, covering the nose and mouth of the child. When the child demonstrates correct technique inhaling directly from the mouthpiece of the spacer, the face mask can be removed, thus decreasing the dead space.28
The spacer should be cleaned with lukewarm soapy water, separating it from the face mask, disassembling the chamber according to the directions of the manufacturer. The chamber (and mask) should be left soaking in the soapy water for a few minutes and then rinsed with lukewarm fresh water. The chamber should be left to air dry in a horizontal position until fully dry, as opposed to wiping it, to minimise static electricity. Washing at high temperatures or with harsh chemicals is not recommended and can damage the spacer. Users need to read the directions for the cleaning and maintenance for each spacer and manufacturer, in addition to periodically reviewing the condition of the chamber and valves, with replacement recommended when it is no longer good. In the case of spacers made of plastic, yearly replacement is recommended. In the selection of spacers, a minimal electrostatic charge and ease of cleaning should be prioritised.
In health care facilities, patients should ideally bring their own spacers for personal use. If the reutilization of spacers is required in a facility, thorough cleaning and disinfection should be performed after each use, following the directions of the manufacturer and the protocols of the facility. An enzymatic detergent and lukewarm water may be used, followed, after rinsing, by immersion in a disinfectant solution.
There are different types of spacers. Providers must know the characteristics and properties of each. A chamber length of 14–28cm is ideal for producing an optimal particle distribution (mass median aerodynamic diameter [MMAD] of 1−5μm), the half-life of which depends on the material the spacer is made of. One of the most relevant characteristics to be aware of is the material of the spacer in order to know whether it is antistatic. If it builds up static, some of the medication particles will adhere to the walls of the chamber, and a lesser amount will be delivered to the airway of the child. This is the reason for priming the spacer prior to using the inhaler (pressing several times on the canister prior to administration of the drug to the child) or washing the spacer (with mild detergent, rinsing with water to prevent inhalation of detergent particles and letting it air dry without wiping it), as recommended for spacers that do not have a low electrostatic charge.28 The volume of spacers varies, and it is important to know that chambers of 150–200mL are considered appropriate for all ages.
It is recommended that spacers have one-way valves that open with minimum effort to allow inhalation of the aerosol. The valve would then close during exhalation so that the remaining medicine stays within the chamber and can be delivered in the following inhalation. Ideally, both valves in the spacer (inhalation/exhalation) would be one-way. In young children, it is important to use spacers with low-resistance valves and to ensure that they can move with the low tidal volumes and inspiratory flow rates of these patients.28,29
It is recommended that the patient inhales through the spacer immediately after the actuation, as any delay decreases the amount of medication that reaches the lungs. The inhaler should be pressed once per inhalation through the spacer, allowing time for the child to breathe through it. There are two inhalation methods using a spacer: with tidal breathing (child breathing normally after each actuation) and single maximal inhalation with breath hold (the child takes a deep breath after the actuation, holding it for approximately 10s). Either technique should be used based on the degree of cooperation of the child. Ideally, the child should be trained on the latter technique before switching to a dry powder inhaler. The ideal inhalation position is for the child to be alert and upright (standing or held sitting on a lap) to allow adequate expansion of the chest and with the inhaler perpendicular to the child’s chest.
In the case of the tidal breathing technique, when it comes to the number of breaths that should be performed, current recommendations indicate that 2–3 breaths, if the spacer is small, or 3–4 breaths, if the spacer is large, are sufficient for older children. Infants and children under 2 years should complete 5–6 breaths to ensure that they inhale all the medication contained in the spacer.29
It is important to known whether a given spacer is universal and compatible with every pressurized MDI and to ensure that the prescribed medication fits well in the spacer used by the patient.
Dry powder inhalersDry powder inhalers (DPIs) are devices in which the medication is housed in a capsule that is usually shaped as a blister. These devices contain the drug in dry powder particles smaller than 5μm, in some cases added to larger carrier particles (lactose or glucose) so that, on impact with the oropharynx, it is possible to perceive that the drug is being delivered. These devices require a minimum inspiratory flow rate of 30L/minute to be actuated, so they can only be used in older children once adequate technique is verified.
There are MDIs containing multiple doses (the most commonly used type) and MDIs containing a single dose (in which the active ingredient is within a capsule and delivery requires a high peak inspiratory pressure). There is a wide variety of designs (Easyhaler, Turbuhaler, Accuhaler, Ellipta…), each of which requires a specific inhaler technique. In essence, the general technique could be summarised thus: opening the container, taking a full expiration, loading the dose (by twisting the base, pressing a button or tab, or directly opening the container), fitting the inhaler in the mouth and creating a tight seal with the lips, performing a deep, long inspiration and then holding the breath for approximately 10s. Afterward, the inhaler is removed from the mouth and the air exhaled through the nose. Some devices, like the Easyhaler, must be shaken before use.
All inhalers are effective as long as the technique is correct. The selection of a particular type should be based on the age and maturity of the child, the preferences of the user, the cost, inhaler/spacer compatibility and, most importantly, the ability of the child to use the inhaler correctly.
When it comes to DPIs, the inspiratory capacity of the child must also be taken into account, as most of these devices require a minimum inspiratory flow rate of 30L/minute.28,29 Different tools are available to assess inspiratory flow rates at the office before prescribing a DPI. For example, replica inhalers with inspiratory flow whistles or inspiratory flow meters are portable and easy to use devices that can be used in clinical settings to assess the inspiratory capacity of each patient and, based on the results, select a device that the patient can use.
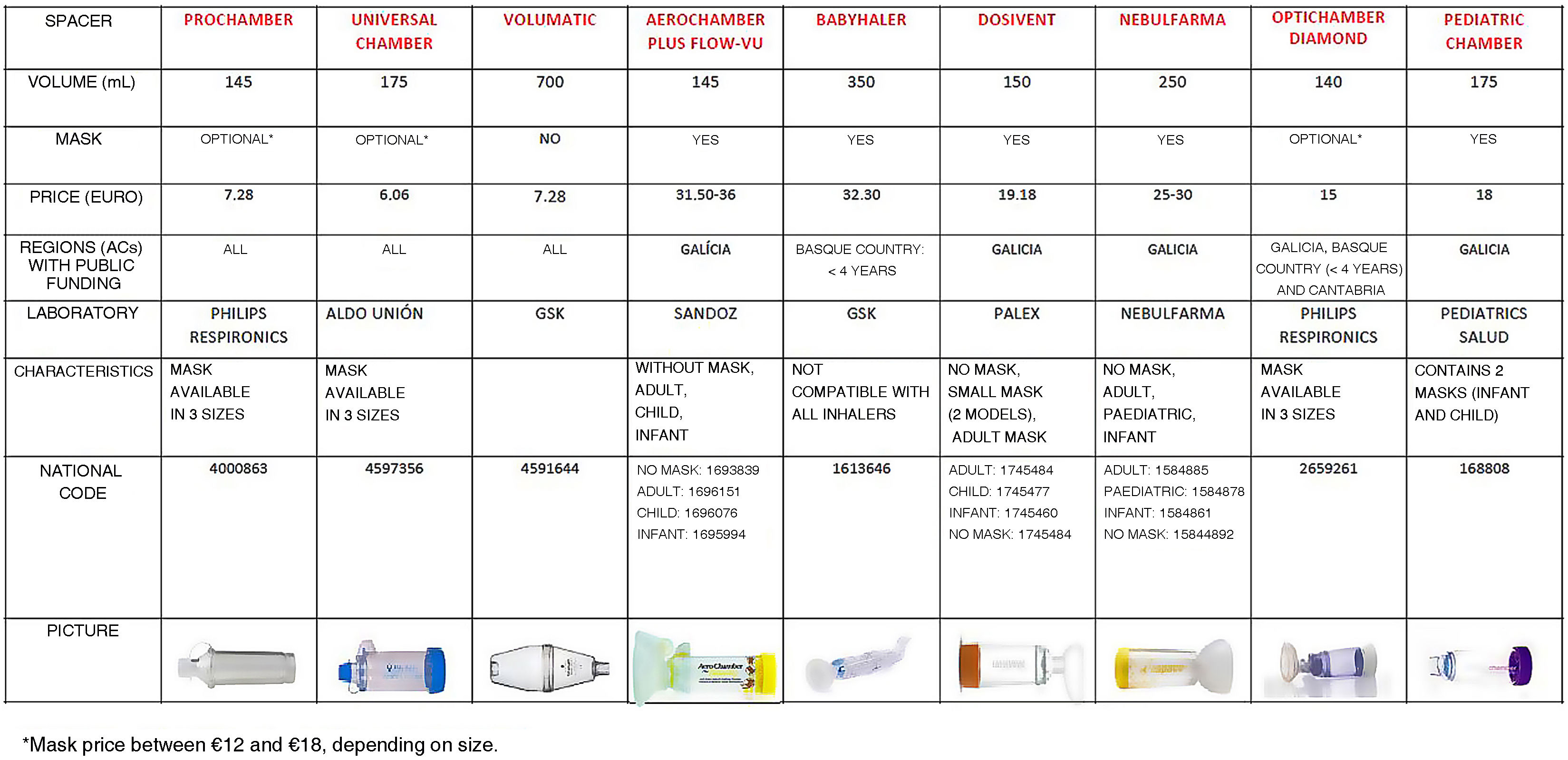
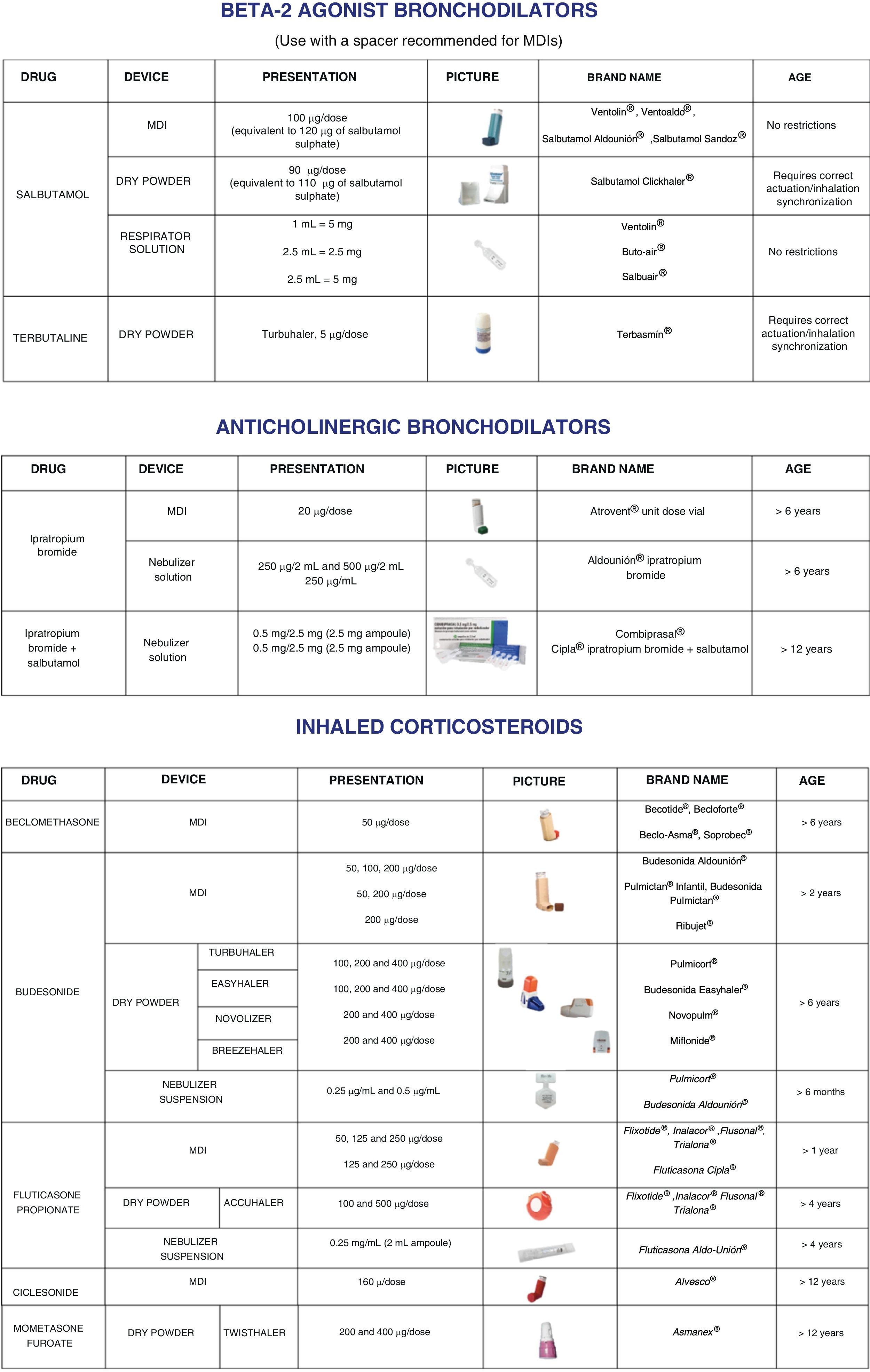
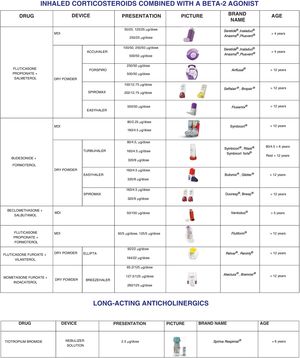
Issued documentsThe updated REGAP review includes 2 tables with pictures that summarise the main characteristics of the most widely used spacers and medication inhalers in paediatric care available in Spain as of January 2023. This document will be updated each year to help health care providers stay informed and up to date about the different treatment options. The next review will start halfway through 2024 and the updated tables will be published in the websites of the different paediatric societies that form the REGAP.
The review is summarised in two documents in table format:
- •
Spacer document: presenting the most widely used spacers in Spain with their main characteristics, size, brand name, domestic code, funding, price and a photograph of the product (Fig. 1).
- •
Inhaled medication document: presenting the asthma medications used most frequently in paediatric patients grouped by type of drug: corticosteroids, short-acting bronchodilators, combination medications (including combinations of corticosteroids with long- or short-acting bronchodilators) and anticholinergics. It also provides information on the different types of devices available for delivery of the medication, the dosage, age range for which it is currently approved, brand name and photographs of the available devices containing the medication (Fig. 2).
The documents can be obtained by printing the files published in the websites of the different scientific societies (https://www.aeped.es/noticias/revision-regap-medicacion-inhalada-y-camaras-inhalacion-asma). Access is free and there are no restrictions or copyrights, so the material can be printed and used for teaching, as an aid in the clinic or as any professional may see fit. We hope that this tool proves useful and practical and helps professionals stay updated regarding currently available inhaled medications, thus contributing to improving the care of patients with asthma.
Conflicts of interestThe authors have no conflicts of interest to declare.