Viral respiratory infections cause major morbidity and mortality in preterm infants. We have performed a prospective study in our neonatal intensive care unit (NICU) to determine the incidence of respiratory infections, their impact and the epidemiology and outcome in high risk neonates.
Patients and methodsFrom September 2011 to May 2013 a prospective study was conducted in all preterm infants <32 weeks gestational age and in all term newborns admitted to NICU for any pathology that was anticipated to have an admission exceeding two weeks. A nasopharyngeal aspirate (NPA) was collected the first day of life and weekly until discharge for virologic study with polymerase chain reaction. When these babies presented respiratory symptoms a new NPA was collected at this moment. A clinical form was filled by the physician.
ResultsA total of 60 infants were analysed: 30 (50%) had a gestational age <32 weeks and 36 (60%) weighed less than 1500g. We collected a total of 256 nasopharyngeal aspirate samples, 24 of them being positive (9.3%). These 24 positive samples corresponded to 13 infants in our cohort (21.6% of the patients). Of them, 9 were symptomatic and had 11 episodes of infection (2 patients had two different episodes with negative control between them). The most frequently identified virus was rhinovirus in (19) 79% of cases. The most frequent clinical data was the presence or increase in apneas (75%) and the need for oxygenotherapy.
ConclusionsHRV infections are prevalent in the NICU, and preterm infants have a high risk of infections with clinical relevance.
Las infecciones virales respiratorias son causa de importante morbimortalidad en recién nacidos prematuros. Hemos realizado un estudio prospectivo en nuestra unidad de cuidados intensivos neonatales (UCIN) para determinar la incidencia de infecciones respiratorias, su impacto, epidemiología y pronóstico en neonatos de alto riesgo.
Pacientes y métodosEstudio prospectivo realizado entre septiembre del 2011 y mayo del 2013 entre todos los recién nacidos < 32 semanas de edad gestacional y aquellos niños cuya patología pudiera dar lugar a pensar en un ingreso superior a las 2 semanas. Se recogieron aspirados nasofaríngeos (ANF) el primer día de vida y semanalmente hasta el alta para estudio virológico mediante reacción en cadena de polimerasa. En los casos en los que los niños presentaban síntomas respiratorios, se procedió a recoger un nuevo ANF. El pediatra cumplimentó un cuestionario con los datos clínicos.
ResultadosSe estudió a 60 niños; 30 (50%) de ellos con una edad gestacional <32 semanas y 36 (60%) con un peso <1.500g. Se recogió un total de 256 ANF, 24 de los cuales resultaron positivos (9,3%). Estas 24 muestras positivas correspondieron solo a 13 niños (21,6% de los pacientes). De ellos, 9 resultaron sintomáticos y presentaron 11 episodios de infección (2 pacientes experimentaron 2 episodios diferentes con control negativo entre ellos). El virus más frecuentemente identificado – el 79% de las muestras (19) – fue el rinovirus (RV). El dato clínico más frecuente fue la presencia o incremento de apneas (75%) y la necesidad de oxigenoterapia.
ConclusionesLas infecciones por RV son frecuentes en la UCIN y los recién nacidos pretérmino tienen un alto riesgo de presentar infecciones de relevancia clínica.
Viral respiratory infections are transmitted from person to person. Many of the viruses that cause them are carried asymptomatically in the nasopharynx1 and symptoms may not show until several days later. Although these diseases are mild in most cases, newborns, and especially those born preterm or with low birth weight, are at high risk of respiratory tract infection with severe symptoms such as respiratory distress, apnoea or haemodynamic instability. These symptoms often cannot be distinguished from symptoms caused by bacterial infections or other diseases associated to prematurity, such as enterocolitis, nosocomial sepsis or apnoea of prematurity, so respiratory viruses are not the only causative agents under consideration. Yet, we know that common viral respiratory tract infections, such as infection by respiratory syncytial virus (RSV), cause considerable morbidity and mortality in preterm patients as well as severe disease outbreaks in neonatal intensive care units (NICUs).2,3 In addition to classical viruses like RSV and influenza viruses, rhinovirus (RV), human metapneumovirus (hMPV), coronavirus (CoV) and human bocavirus (hBoV) play an increasingly important role in respiratory tract infections in infants. Very little is known about their role in neonatal units,4,5 although we have demonstrated that they are associated with relevant pathology in our unit.6,7
Neonatal units devote considerable effort to set up measures to prevent infection, such as the use of hygiene measures of proved effectiveness by any staff that comes in contact with the infants: applying alcohol gel before and after manipulating the child, wearing gloves, frequent handwashing, prevention of catheter-related sepsis by monitoring the catheter and withdrawing it as early as possible, and the prudent use of antibiotics.
Neonatal units have changed dramatically in recent years, offering a more holistic care to the neonate and his or her family and a more humane approach that is manifested in the full participation of parents in the care of the child at any time of day or night; that is, an open-door policy. Educating the parents on the hygiene protocols before and during their stay in the unit allows them to be part of the team that cares for the infant. Our NICU (which belongs to a secondary hospital that attends 1800 births a year) has an open-door policy that allows parents to be involved in the infant's care.
Our aim was to assess the presence (symptomatic and asymptomatic) of 16 respiratory viruses in term and preterm neonates admitted to the NICU, and to describe the associated clinical manifestations.
Patients and methodsWe performed a prospective cohort study at the Hospital Severo Ochoa (Leganés, Madrid) to assess the incidence, aetiology and clinical characteristics of viral respiratory infections in neonates that required admission to the NICU for 2 or more weeks. Patients were enrolled between November 2011 and May 2013. The study was funded by grant number 09/00246 of the Fondo de Investigaciones Sanitarias and approved by the Medical Ethics Committee of the Hospital Severo Ochoa. The parents signed an informed consent form before patients were included in the study.
We collected a nasopharyngeal aspirate (NPA) sample the first day of life and weekly until discharge. When infants developed respiratory symptoms such as cough, respiratory distress, rhinorrhoea and longer than usual apnoeic pauses with or without fever, an additional NPA sample was collected at the moment. The neonatologist filled out a clinical form for each episode.
The NPA specimens were sent to the Unidad de Virus Respiratorios y Gripe (Unit of Respiratory Viruses and Influenza) of the Centro Nacional de Gripe (National Influenza Centre) of the World Health Organisation, the Instituto de Salud Carlos III, in Madrid, Spain. This unit subjected the specimens to three nested real-time polymerase chain reaction (RT-PCR) assays for the detection of a total of 16 respiratory viruses, as reported in previous publications.8–10
We have expressed discrete variables as percentages and continuous variables as mean±standard deviation (SD). We compared the variables corresponding to clinical and laboratory characteristics by means of Student's t test, the Mann–Whitney U test, the χ2 test and Fisher's exact test. We set the level of statistical significance (for two-tailed tests) at P<.05. The statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 13.0.
ResultsThe study included 66 infants (all but one born preterm), six of which (9%) were withdrawn from the study by their parents during followup. We analysed the data for a total of 60 infants: 33 (55%) were female; 30 (50%) had a gestational age below 32 weeks; and 36 (60%) weighed less than 1500g. Mechanical ventilation was required by 41.7% of the patients (mean duration±SD, 2.31±1.73 days) and continuous positive airway pressure (CPAP) by 31.7% (mean duration±SD, 2.45±1.74h).
A total of 256 NPA samples were collected, and 24 tested positive (9.3%); none of the positive specimens had been collected in the first day of life. The virus identified most frequently was RV, detected in 19 (79%) of the positive samples, followed by adenovirus (2 cases), CoV (3 cases) and hMPV (1 case). One patient had a RV and CoV coinfection. There were no cases of RSV or influenza. The positive NPA specimens were obtained at a mean of 35±21 days (range, 8–68; median, 30). We observed a higher frequency of samples positive for respiratory viruses in patients younger than 32 weeks and with weights below 1500g (P=.05 and P<.001, respectively).
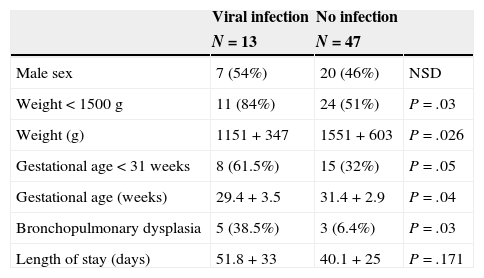
The 24 positive samples corresponded to 13 infants (21.6% of the patients), of which 9 (69%) developed symptoms, with a total 11 infectious episodes (2 patients had 2 separate episodes with a negative test result in between). Table 1 shows the clinical characteristics of the episodes of respiratory infection. The symptoms found most frequently were the presence or greater number of apnoeic episodes (75%) and the need for oxygen therapy. None of the patients required mechanical ventilation, and only one patient received noninvasive ventilation. Fever occurred in 45% of the infectious episodes.
Clinical characteristics of patients with and without viral respiratory infection (symptomatic or asymptomatic).
| Viral infection | No infection | ||
|---|---|---|---|
| N=13 | N=47 | ||
| Male sex | 7 (54%) | 20 (46%) | NSD |
| Weight<1500g | 11 (84%) | 24 (51%) | P=.03 |
| Weight (g) | 1151+347 | 1551+603 | P=.026 |
| Gestational age<31 weeks | 8 (61.5%) | 15 (32%) | P=.05 |
| Gestational age (weeks) | 29.4+3.5 | 31.4+2.9 | P=.04 |
| Bronchopulmonary dysplasia | 5 (38.5%) | 3 (6.4%) | P=.03 |
| Length of stay (days) | 51.8+33 | 40.1+25 | P=.171 |
| N=11 | |
|---|---|
| Clinical data (signs and symptoms) | |
| Greater number of apnoea episodes | 8 (72%) |
| Rhinorrhoea | 7 (63%) |
| Fever | 5 (45%) |
| Cough | 1 (9%) |
| Respiratory support | |
| Environmental oxygen | 9 (81%) (maximum FiO2, 0.3) |
| Nasal cannula | 5 (45%) |
| CPAP | 1(9%) |
| CMV | 0 (0%) |
| None | 2 (18%) |
CMV: conventional mechanical ventilation; CPAP: continuous positive airway pressure; NSD: no significant differences.
Laboratory analyses were performed in 7 (64%) of the 11 infectious episodes; only one patient had leukocytosis (32,000/mL). Blood cultures were performed in 4 (36%) cases, and the results were negative for all. Antibiotic therapy was initiated in one patient for suspected sepsis. Five infants underwent chest radiographs, and atelectasis was found in one. All patients recovered.
Four of the children with positive samples did not develop clinical symptoms (three had RV 3 and one CoV OC43). One of the symptomatic infants had prolonged shedding of RV for 8 weeks. No tests were performed on the healthcare staff or the parents.
Table 1 compares the clinical data of the patients, (symptomatic and asymptomatic), with obtaining a positive result in the viral assays. Of the 13 infants that had a positive viral isolate, 5 (38%) developed bronchopulmonary dysplasia. One of them had an asymptomatic infection by CoV OC43 and the other 4 symptomatic infections by RV or adenovirus. Of the children that did not have a positive viral isolate, 3 (6.4%) were diagnosed with bronchopulmonary dysplasia (P=.009).
DiscussionNosocomial infections are among the major causes of morbidity, prolonged hospitalisation and mortality in neonates, especially in those born preterm. Most of the scientific literature focuses on bacterial or fungal infections and does not consider respiratory viruses, except for RSV.11 We present the results of a prospective cohort study in 16 viral respiratory infections conducted in the NICU of a secondary hospital. Viral respiratory infections, especially those by RV, are fairly frequent in the neonatal unit and are associated with episodes of apnoea and the need for respiratory support, especially in preterm newborns of less than 32 weeks of gestational age or with weights below 1500g.
The advent of PCR techniques has revealed the involvement in lower respiratory tract infections in children, and that this is one of the most important viruses overall in the epidemiology of respiratory infections. Various groups have recently identified RV as the causative agent of respiratory infection outbreaks in neonatal units. Reid et al.5 described an outbreak of infection by RV type C in 7 infants in a paediatric and neonatal intensive care unit, 5 of which had clinically relevant episodes of apnoea and required respiratory support or oxygen therapy. Van Piggelen et al.12 described 7 severe nosocomial infections associated to RV in the NICU over a period of 5 years, all of which were associated with respiratory distress and required ventilatory support. In both studies, respiratory infections were suspected and a viral aetiology was actively explored. The clinical data of these two studies are similar to those obtained in our cohort.
However, our data show that respiratory viruses are responsible for a considerable number of disease episodes that worsen respiratory status and that are attributed to prematurity when in fact they are due to viral infections. We only found a similar study that focused on detecting unrecognised respiratory viral infections in preterm neonates admitted after delivery. In this prospective study, which had a design similar to ours, Bennett et al.13 observed that 52% of the 60 preterm neonates tested for viral detection had positive results during their stay. This group of neonates had longer lengths of stay, prolonged respiratory support, and a higher incidence of bronchopulmonary dysplasia. In our patients, the proportion of bronchopulmonary dysplasia was also greater in infants in whom a virus had been detected, but the group of children that tested negative for viruses had a greater gestational age, a circumstance that may lead to misinterpretation of the results. The proportions of the viruses detected by Bennett et al. differed somewhat from ours, with a high prevalence of RSV, parainfluenza virus and hMPV, especially in the winter. Rhinovirus was detected in only 27% of the patients. The lower incidence of viral infections by RSV or influenza in our group may have been due to our meticulous adherence to the preventive measures against nosocomial infections.
We agree with Bennett in thinking that while there are descriptions of outbreaks of viral respiratory infections in NICUs, these studies substantiate the importance of systematic surveillance for detecting infections that would otherwise not be recognised. Preterm infants may present few or atypical symptoms, and the detection of viral infections may have profound clinical consequences. Our study was limited by the small number of patients included in it, so it is important that other prospective studies are performed to elucidate the actual role of viral respiratory infections in neonatal units.
We did not explore the sources of the infections, but the infants only had contact with their parents and the healthcare staff. And while we presumably adhere rigorously to preventive measures against nosocomial infections including the use of gloves, handwashing before and after each contact with a patient, and having any individual with respiratory symptoms wear a mask, transmission of respiratory viruses does occur and we should explore new preventive strategies.
In short, we found that RV may be the cause of respiratory infections in preterm neonates during their stay in the NICU, and that preterm infants are at high risk of acquiring clinically significant infections of this kind. Viral respiratory infections should be ruled out in infants with rhinorrhoea, apnoea, high oxygen requirements and clinical suspicion of sepsis. We must apply rigorous measures for infection prevention and possibly introduce additional hygiene measures.
FundingThis study has been funded by the Instituto Nacional de Salud de España (ISCIII, Fondo de Investigaciones Sanitarias), PI 09/00246 and PI 12/0129.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Gonzalez-Carrasco E, Calvo C, García-García ML, Beato M, Muñoz-Archidona C, Pozo F, et al. Infecciones virales de las vías respiratorias en la Unidad de Cuidados Intensivos Neonatales. An Pediatr (Barc). 2015;82:242–246.