A 17-day-old neonate was admitted with a diffuse erythematous rash and peeling skin. The infant had been well until day 13 post birth, when a preauricular blister appeared. The patient had been born at 35 weeks via caesarean section after an uncomplicated pregnancy, resided in a hygienic environment and had no family history of cutaneous disorders.
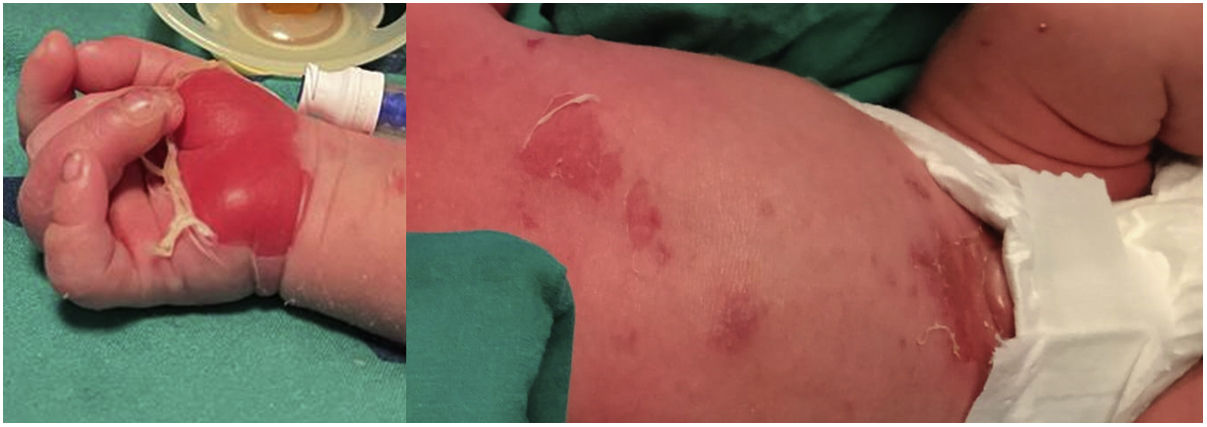
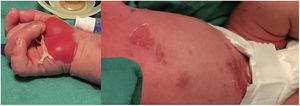
The newborn presented with fever, crusty yellow sores in the face, conjunctivitis, purulent umbilical discharge (Fig. 1), and a positive Nikolsky sign1 (Fig. 2) on examination. The oral mucosa was spared. The C-reactive protein level was elevated (56mg/L). These features led to suspicion of staphylococcal scalded skin syndrome (SSSS), prompting initiation of empirical treatment with intravenous flucloxacillin. Methicillin-resistant Staphylococcus aureus (MRSA) was isolated from skin and conjunctiva/umbilicus cultures, while the blood cultures were negative. Both parents tested negative for MRSA.
Flucloxacillin was discontinued and intravenous vancomycin administered for 14 days, with addition of topical mupirocin as an adjuvant in an attempt to eradicate colonization.2 After 3 days of therapy, the patient was afebrile and the skin lesions showed signs of healing. The newborn was discharged with intact skin (Fig. 3), and no recurrences have been documented.
Staphylococcal scalded skin syndrome is a rare, life-threatening neonatal condition. Early recognition prevents complications, guiding effective treatment.1 Neonatal MRSA outbreaks often result from transmission from asymptomatic carriers and require MRSA screening.3
Previous presentation: Northern Interhospital Pediatric Cycle held at the Ordem dos Médicos (Porto, Portugal), February 17, 2023.