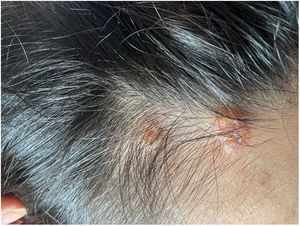
A healthy female adolescent aged 14 years - with a family history of psoriasis presented to the paediatric emergency department with pruritic, intermittent and refractory mucocutaneous lesions with onset 3 months before. Additionally, the patient reported having lost 10% of her body weight and secondary amenorrhea. The physical examination revealed oral mucosa ulcerations, lip oedema (Fig. 1), scalp lesions (Fig. 2) and scattered vesiculobullous lesions with serous discharge, several with secondary impetiginization (Fig. 3).
During hospitalization, the blood tests detected eosinophilia (1800/µL) and an elevated erythrocyte sedimentation rate. Examination of a biopsy scalp lesion specimen revealed pustular folliculitis with eosinophilic infiltration. Hypereosinophilic syndrome (HS), was considered as a possible diagnosis, a disorder characterized by peripheral blood eosinophilia with end-organ damage attributable to eosinophilia after ruling out other causes.1,2
In light of this suspicion, a digestive endoscopy was performed that revealed a continuously and diffusely oedematous, friable mucosa with complete obliteration of the vascular pattern in the terminal ileum and colon. The findings of the biopsy confirmed ileitis, colitis and proctitis marked by eosinophilic infiltration. No other causes of eosinophilia or systemic involvement were identified.
Subsequently, empirical therapy was administered, consisting of oral prednisolone and topical betamethasone, resulting in significant clinical improvement.
This clinical case aims to raise awareness of the atypical presentations of HS, a rare and potentially severe disease that is often underdiagnosed.
Presentación oral previa: Este caso fue presentado en el Ciclo Pediátrico Interhospitalario del Norte (Ordem dos Médicos), 27 de enero de 2023.