To analyse the clinical and epidemiological characteristics of children who are attended in Emergency Departments (EDs) for an unintentional injury in Spain.
MethodsMulticentre case series with prospective data collection conducted during 12 months in the ED of 11 hospitals belonging to the Spanish Paediatric Emergency Research Group. Data were collected between September 2014 and January 2015, continuing for one year in all paediatric EDs, and included children between 0 and 16 years old seen for an unintentional injury.
ResultsA total of 10,175 episodes were recorded during the study, of which 1941 were due to unintentional injuries (19.1%, 95% CI: 18.3%–19.8%), and 1673 of these were included in the study. Falling, direct injuries, and injuries due to sports activities represented more than 80%, with significant variations in the injuries mechanism observed in different age groups. More than occurred at home or school. About 40% of the unintentional injuries were not witnessed by an adult. The most frequent diagnosis was limb trauma (63.0%), with a fracture being observed in 242 (14.4% of unintentional injuries). As regards fractures, 34 (2.0%) were admitted to hospital, with 21 (61.8%) for surgical reduction of the fracture. No deaths were recorded in the first 24h.
ConclusionsUnintentional injuries constitute a very common reason for consultation in EDs in Spain. The circumstances surrounding the unintentional injuries should be considered, in order to develop preventive measures and to improve the training of people involved in the care of these children.
Analizar las características clínico-epidemiológicas de los niños que consultan en urgencias por una lesión no intencionada (LNI) en España.
MétodosSerie de casos multicéntrica con recogida de datos prospectiva desarrollada durante 12 meses, en los servicios de urgencias pediátricos (SUP) de 11 hospitales pertenecientes a la Red de Investigación de la Sociedad Española de Urgencias Pediátricas. La recogida de datos comenzó entre septiembre de 2014 y enero de 2015, continuando durante un año en todos los servicios de urgencias pediátricos, incluyéndose los niños de 0 a 16 años que consultaron por LNI.
ResultadosDurante el estudio se registraron 10.175 episodios, de los que 1.941 correspondieron a LNI (19,1%, IC 95%: 18,3-19,8%), incluyéndose 1.673 en el estudio. Las caídas, traumatismos directos y las lesiones derivadas de actividades deportivas constituyeron más del 80%, observándose variaciones significativas del mecanismo lesional en diferentes grupos de edad. Más de la mitad se produjeron en casa o en el colegio. En el 39% la LNI no fue presenciada por un adulto. El diagnóstico más frecuente fue traumatismo de extremidades (63,0%), objetivándose una fractura en 242 (14,4% de las LNI). Ingresaron 34 (2,0%) pacientes, sobre todo para reducción quirúrgica de fracturas (21, el 61,8% del total de ingresos). No se registraron fallecimientos en las primeras 24h.
ConclusionesLas LNI constituyen un motivo muy frecuente de consulta en urgencias en España. El conocimiento de las circunstancias que rodean a estas LNI ayudaría a desarrollar medidas preventivas adecuadas y mejorar la capacitación de las personas, sanitarias o no, que pueden participar en la atención a estos niños.
Each year, nearly 37 million people in the European Union seek care for injuries in emergency departments; of all these injuries, 14.1% require hospital admission and 0.6% result in death.1 In the paediatric population, more than two thirds of these deaths are due to unintentional injuries (UIs), which are injuries in which the harmful outcome was not sought or results from the physical energy in the environment. These UIs generate millions of visits per year to European hospitals.2 Thus, every year 1 in 10 children in the European Union experiences an injury that requires urgent medical attention.2
The most frequent mechanisms of death due to UIs in children are road traffic accidents, followed by drowning, poisoning, thermal injuries and falls.3 Although most injuries can be treated, recent studies suggest that the impairment that may result from even mild injuries can affect the quality of life of a child for 2 to 3 years.4
More importantly, many of these UIs are preventable,3 while the costs associated with their treatment are high.4
In order to develop effective preventive measures and improve care efficiency, we need to learn the circumstances that surround UIs in our country.
While there is a register of UIs managed at the primary care level,5 there is very little data on the characteristics of paediatric patients that seek emergency care for UIs in Spain.
The aim of the study was to analyse the clinical and epidemiological characteristics of children that seek emergency care for UIs in Spain.
Materials and methodsStudy designWe present a multicentric case series with prospective data collection over a period of 12 months in 11 paediatric emergency departments (PEDs) of secondary and tertiary care hospitals that are part of the Sociedad Española de Urgencias Pediátricas (Spanish Society of Paediatric Emergency Medicine) Research Network (RiSEUP-SPERG).
All participating hospitals included patients over a period of 1 year, starting between September 2014 and January 2015.
Data were collected by means of an online form for every visit to participating PEDs associated to an UI on the 13th of each month between 12:00 am and 12 pm. We chose the 13th of each month because it generally did not coincide with holidays. The physicians that managed the patients entered the data in the form after completing a questionnaire administered to the family members during the patient's stay in the emergency department, and the data entered in the form were submitted automatically to the coordinators of the register, who were responsible for their processing and analysis.
Patients were managed according to existing protocols or the judgement of the physician in charge, and the performance of this study did not modify usual clinical practice.
The study was approved by the clinical research ethics committee of each participating hospital.
To safeguard confidentiality, the database did not include any identifiable information. We obtained written informed consent from the parents or legal guardians of patients aged less than 12 years, and from both the child and the parents or legal guardians of the child when the patient was aged more than 12 years.
Definitions- •
UI: events where the injury occurs in a short period of time (seconds or minutes), the harmful outcome was not sought, or the outcome was the result of normal body functions being blocked by external means.6
- •
Intentional injury: injury resulting from violence, understood, based on the definition of the World Health Organization, as the intentional use of physical force or power, threatened or actual, against oneself, another person, or either a group or community, that either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment or deprivation.7
Children aged 0–16 years that sought care for an UI in any of 11 PEDs of secondary and tertiary care hospitals included in the RiSEUP-SPERG research network.
Six of the 11 PEDs managed patients from birth to their 14th birthday (excluded), 2 PEDs from birth to their 15th birthday (excluded), and the remaining 3 from birth to their 16th birthday (excluded). This reflects the substantial variability that exists in the age limit for receiving care Spanish PEDs.
Exclusion criteria- •
Patients for who we did not obtain informed consent.
- •
Intentional injuries. The intent was assessed by the researchers at each hospital based on the guidelines of the Sociedad Española de Urgencias Pediátricas.8
We collected epidemiologic data (age, sex and personal history), data related to the circumstances surrounding the injury (day of the week, setting, mechanism and whether the injury was witnessed), and data on emergency care (date of service, time elapsed from injury and how the patient was transported to the PED, type of injury, primary diagnosis and death within 24h from the injury).
We grouped the months into seasons as follows: winter (January, February, March); spring (April, May, June); summer (July, August, September), and autumn (October, November, December). We grouped the times of service into morning (8:00 am to 15:00 pm), afternoon (15:00 to 22:00 pm) and night (22:00 pm to 8:00 am).
Statistical analysisWe have summarised categorical variables as absolute frequencies and percentages and calculated the corresponding 95% confidence intervals. We analysed the association between qualitative variables by means of the chi square test or the Fisher exact test.
We created the following age categories: <1 year, 1–4 years, 5–9 years, 10–14 years and 15–16 years.
We performed the statistical analysis with the software SPSS version 21.0. We defined statistical significance as a p-value of less than 0.05.
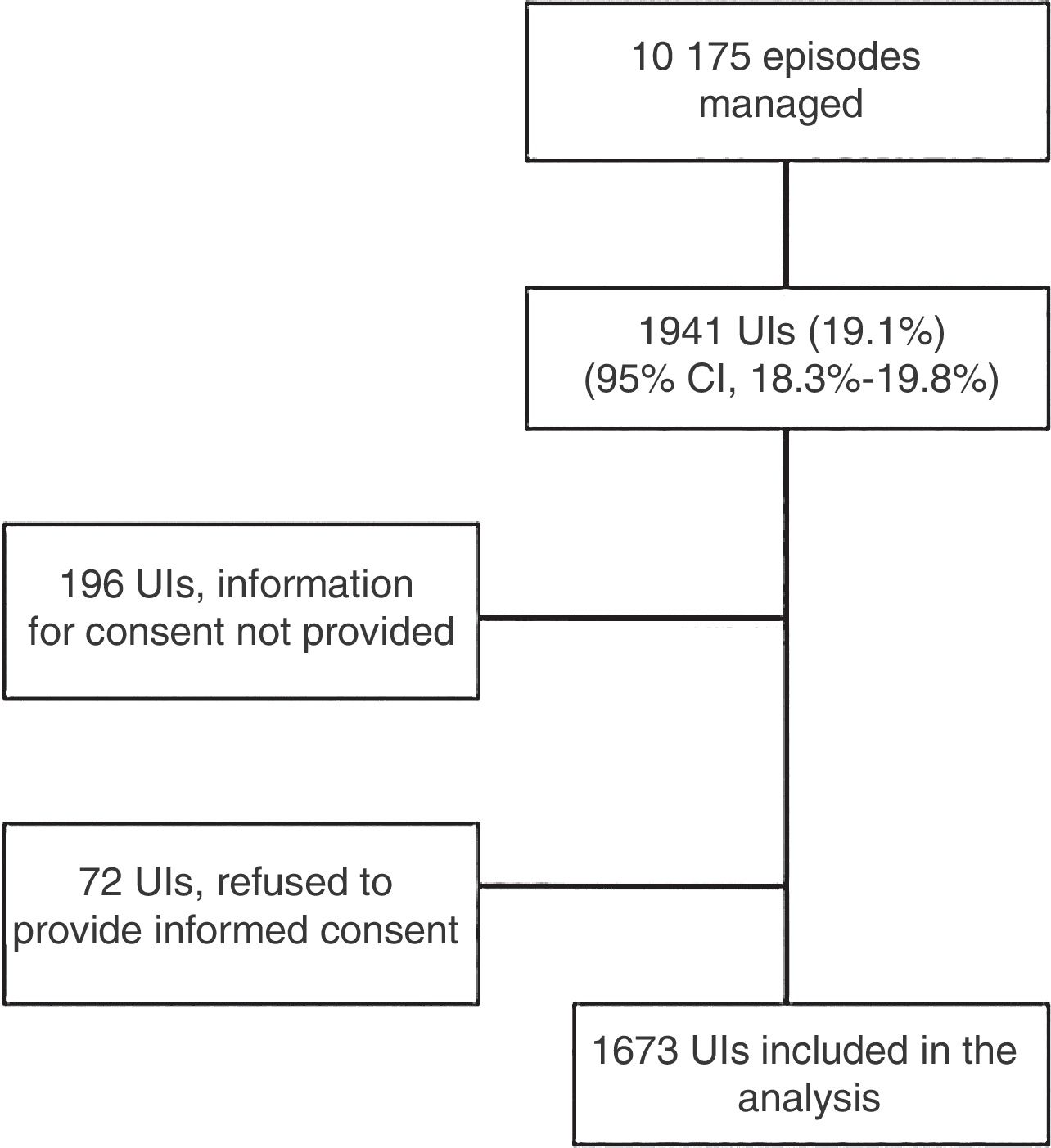
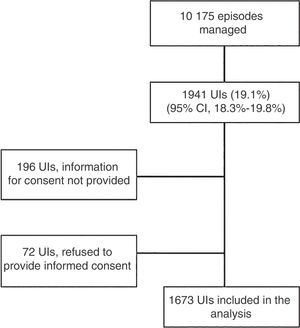
ResultsEpidemiological dataIn the days under study, 10175 cases were managed in the participating PEDs, and 1941 corresponded to children with UIs (19.1%; 95% CI, 18.3%–19.8%) (Fig. 1), of which 1673 were finally included in the study.
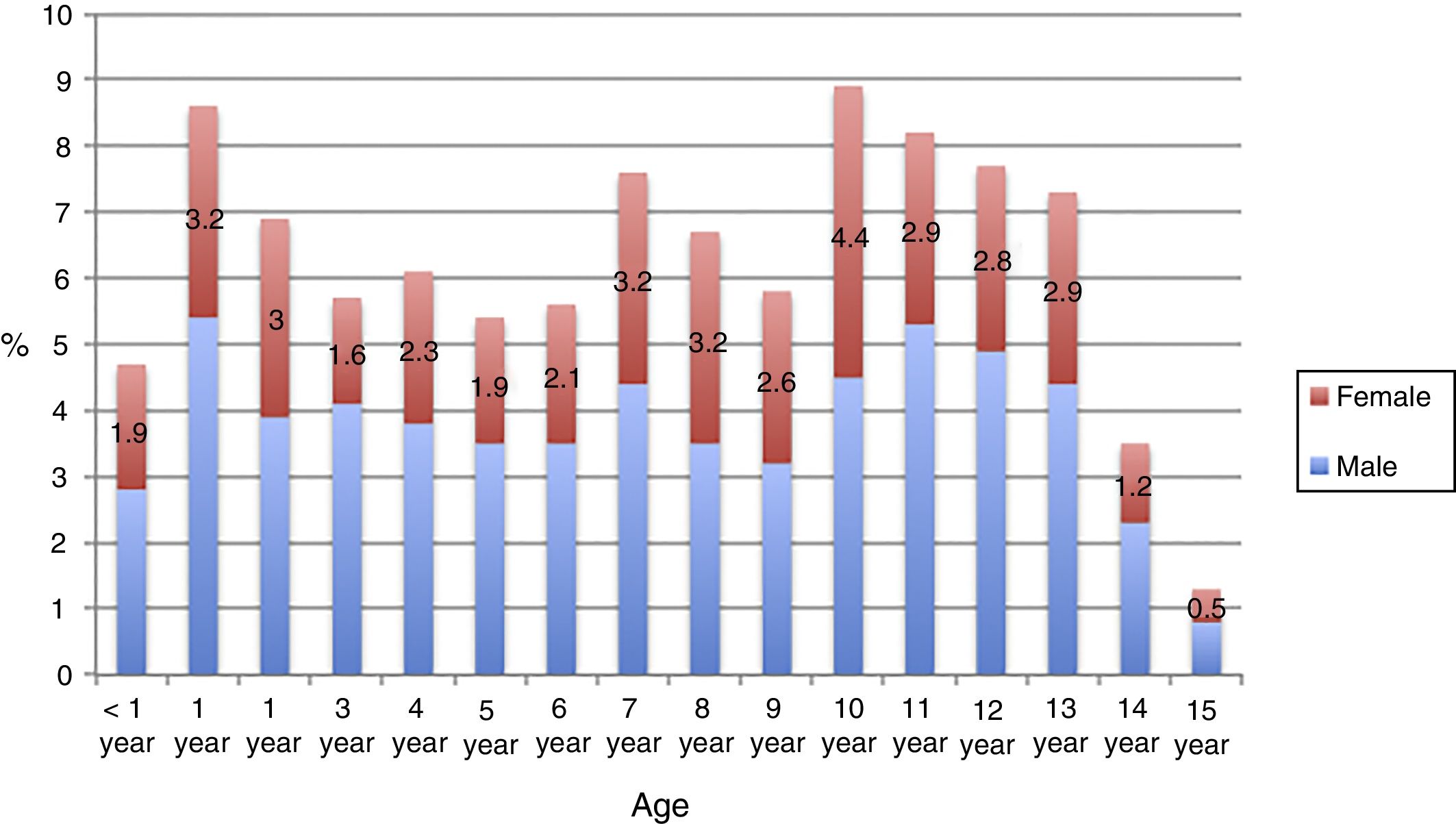
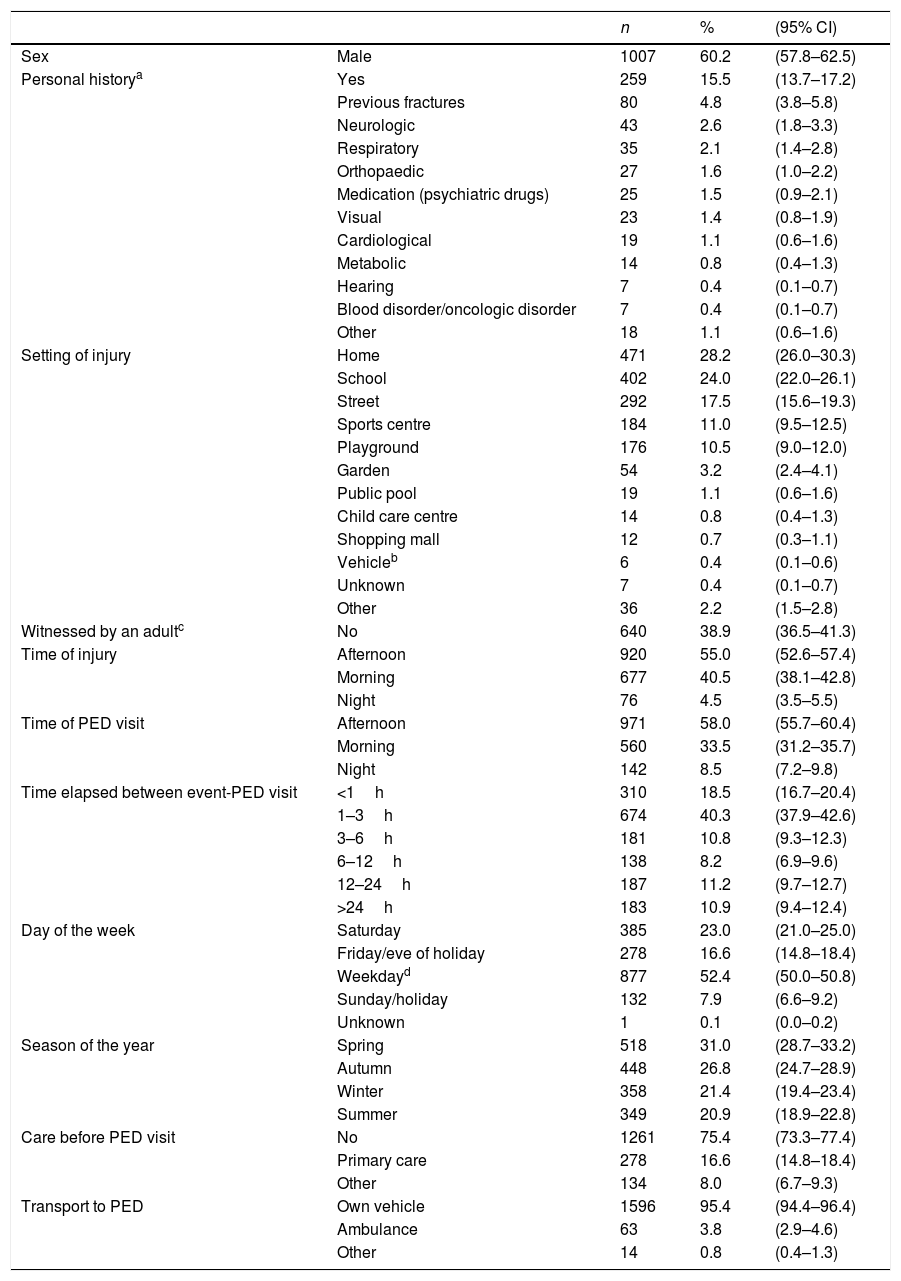
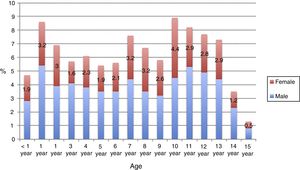
Table 1 presents the general characteristics of the patients, and Fig. 2 the distribution by age and sex.
Epidemiological characteristics of the 1673 patients with unintentional injuries included in the study.
| n | % | (95% CI) | ||
|---|---|---|---|---|
| Sex | Male | 1007 | 60.2 | (57.8–62.5) |
| Personal historya | Yes | 259 | 15.5 | (13.7–17.2) |
| Previous fractures | 80 | 4.8 | (3.8–5.8) | |
| Neurologic | 43 | 2.6 | (1.8–3.3) | |
| Respiratory | 35 | 2.1 | (1.4–2.8) | |
| Orthopaedic | 27 | 1.6 | (1.0–2.2) | |
| Medication (psychiatric drugs) | 25 | 1.5 | (0.9–2.1) | |
| Visual | 23 | 1.4 | (0.8–1.9) | |
| Cardiological | 19 | 1.1 | (0.6–1.6) | |
| Metabolic | 14 | 0.8 | (0.4–1.3) | |
| Hearing | 7 | 0.4 | (0.1–0.7) | |
| Blood disorder/oncologic disorder | 7 | 0.4 | (0.1–0.7) | |
| Other | 18 | 1.1 | (0.6–1.6) | |
| Setting of injury | Home | 471 | 28.2 | (26.0–30.3) |
| School | 402 | 24.0 | (22.0–26.1) | |
| Street | 292 | 17.5 | (15.6–19.3) | |
| Sports centre | 184 | 11.0 | (9.5–12.5) | |
| Playground | 176 | 10.5 | (9.0–12.0) | |
| Garden | 54 | 3.2 | (2.4–4.1) | |
| Public pool | 19 | 1.1 | (0.6–1.6) | |
| Child care centre | 14 | 0.8 | (0.4–1.3) | |
| Shopping mall | 12 | 0.7 | (0.3–1.1) | |
| Vehicleb | 6 | 0.4 | (0.1–0.6) | |
| Unknown | 7 | 0.4 | (0.1–0.7) | |
| Other | 36 | 2.2 | (1.5–2.8) | |
| Witnessed by an adultc | No | 640 | 38.9 | (36.5–41.3) |
| Time of injury | Afternoon | 920 | 55.0 | (52.6–57.4) |
| Morning | 677 | 40.5 | (38.1–42.8) | |
| Night | 76 | 4.5 | (3.5–5.5) | |
| Time of PED visit | Afternoon | 971 | 58.0 | (55.7–60.4) |
| Morning | 560 | 33.5 | (31.2–35.7) | |
| Night | 142 | 8.5 | (7.2–9.8) | |
| Time elapsed between event-PED visit | <1h | 310 | 18.5 | (16.7–20.4) |
| 1–3h | 674 | 40.3 | (37.9–42.6) | |
| 3–6h | 181 | 10.8 | (9.3–12.3) | |
| 6–12h | 138 | 8.2 | (6.9–9.6) | |
| 12–24h | 187 | 11.2 | (9.7–12.7) | |
| >24h | 183 | 10.9 | (9.4–12.4) | |
| Day of the week | Saturday | 385 | 23.0 | (21.0–25.0) |
| Friday/eve of holiday | 278 | 16.6 | (14.8–18.4) | |
| Weekdayd | 877 | 52.4 | (50.0–50.8) | |
| Sunday/holiday | 132 | 7.9 | (6.6–9.2) | |
| Unknown | 1 | 0.1 | (0.0–0.2) | |
| Season of the year | Spring | 518 | 31.0 | (28.7–33.2) |
| Autumn | 448 | 26.8 | (24.7–28.9) | |
| Winter | 358 | 21.4 | (19.4–23.4) | |
| Summer | 349 | 20.9 | (18.9–22.8) | |
| Care before PED visit | No | 1261 | 75.4 | (73.3–77.4) |
| Primary care | 278 | 16.6 | (14.8–18.4) | |
| Other | 134 | 8.0 | (6.7–9.3) | |
| Transport to PED | Own vehicle | 1596 | 95.4 | (94.4–96.4) |
| Ambulance | 63 | 3.8 | (2.9–4.6) | |
| Other | 14 | 0.8 | (0.4–1.3) |
We have expressed data on the main mechanisms of injury as absolute frequencies, percentages and 95% confidence intervals (CIs).
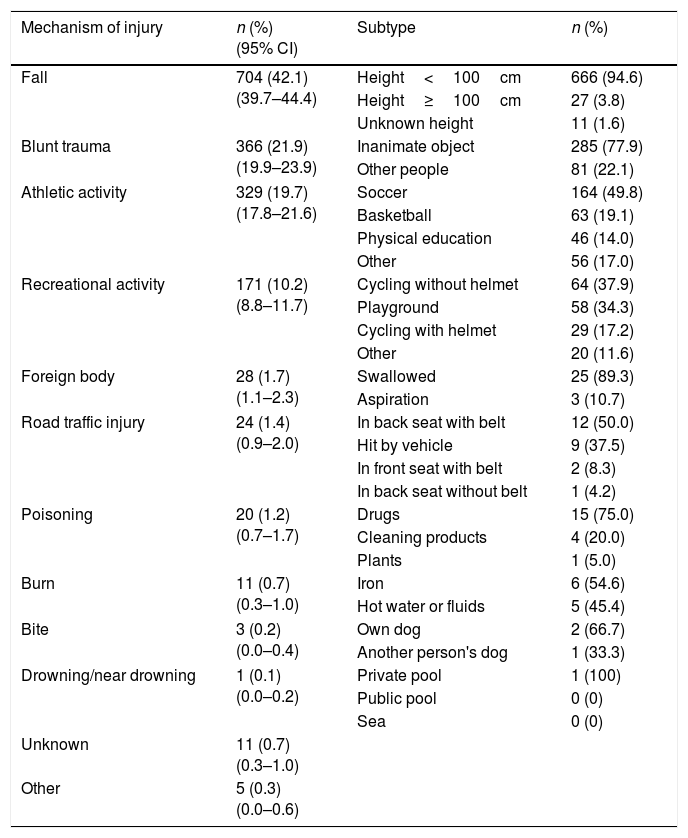
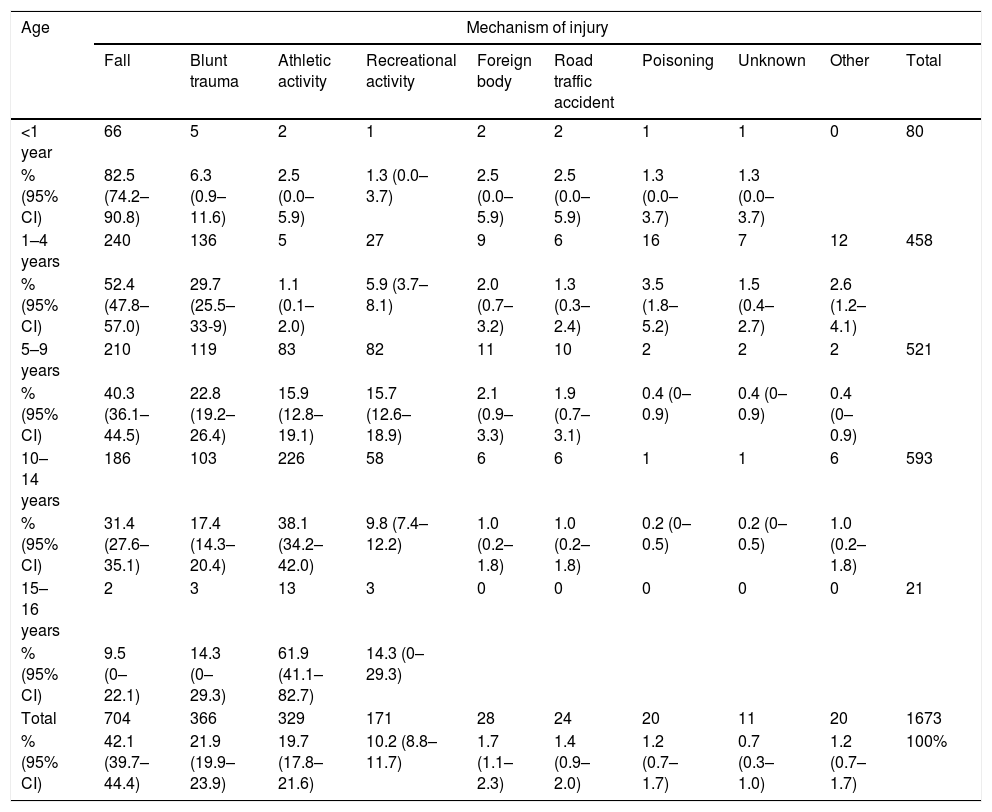
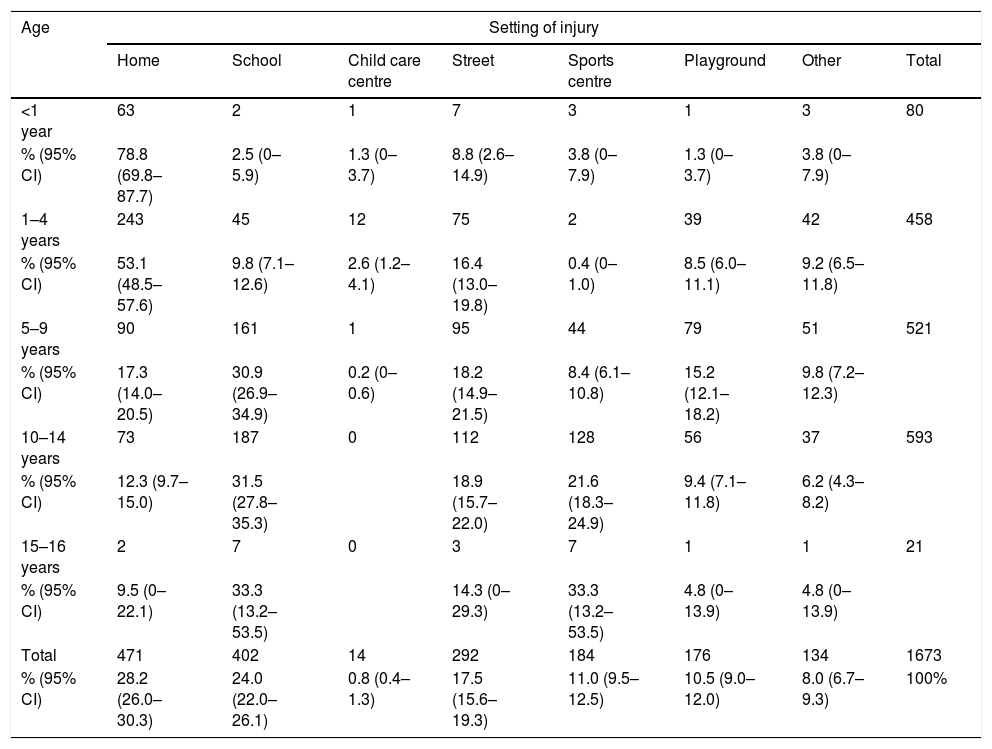
Table 2 presents the most frequently reported mechanisms of injury, and Table 3 the variation in their frequency by age group. There were no significant differences in the mechanisms of injury based on the day of the week, although the percentage of injuries due to recreational activities nearly doubled in summer (16.0%; 95% CI, 12.2%–19.9%) compared to the mean percentage for the other seasons (8.5%; 95% CI, 5.6%–11.5%), while the proportion of injuries due to athletic activities was more frequent in other seasons (21.0%; 95% CI, 16.8%–25.3%) compared to summer (14.9%; 95% CI, 11.2%–18.6%. The setting where the UIs took place varied significantly with age (Table 4). We did not find differences in adult supervision at the time of injury based on age, sex, mechanism of injury, setting of injury, day of the week or season of the year. The setting where fractures occurred most frequently was in a vehicle (33.3%), followed by yards (20.4%) and the street (20.2%). Thus, road traffic accidents (29.2%) and recreational activities (18.7%) were the circumstances associated most frequently with fractures, with no differences between age groups or based on the presence or absence of adult supervision.
Mechanisms of unintentional injury.
| Mechanism of injury | n (%) (95% CI) | Subtype | n (%) |
|---|---|---|---|
| Fall | 704 (42.1) (39.7–44.4) | Height<100cm | 666 (94.6) |
| Height≥100cm | 27 (3.8) | ||
| Unknown height | 11 (1.6) | ||
| Blunt trauma | 366 (21.9) (19.9–23.9) | Inanimate object | 285 (77.9) |
| Other people | 81 (22.1) | ||
| Athletic activity | 329 (19.7) (17.8–21.6) | Soccer | 164 (49.8) |
| Basketball | 63 (19.1) | ||
| Physical education | 46 (14.0) | ||
| Other | 56 (17.0) | ||
| Recreational activity | 171 (10.2) (8.8–11.7) | Cycling without helmet | 64 (37.9) |
| Playground | 58 (34.3) | ||
| Cycling with helmet | 29 (17.2) | ||
| Other | 20 (11.6) | ||
| Foreign body | 28 (1.7) (1.1–2.3) | Swallowed | 25 (89.3) |
| Aspiration | 3 (10.7) | ||
| Road traffic injury | 24 (1.4) (0.9–2.0) | In back seat with belt | 12 (50.0) |
| Hit by vehicle | 9 (37.5) | ||
| In front seat with belt | 2 (8.3) | ||
| In back seat without belt | 1 (4.2) | ||
| Poisoning | 20 (1.2) (0.7–1.7) | Drugs | 15 (75.0) |
| Cleaning products | 4 (20.0) | ||
| Plants | 1 (5.0) | ||
| Burn | 11 (0.7) (0.3–1.0) | Iron | 6 (54.6) |
| Hot water or fluids | 5 (45.4) | ||
| Bite | 3 (0.2) (0.0–0.4) | Own dog | 2 (66.7) |
| Another person's dog | 1 (33.3) | ||
| Drowning/near drowning | 1 (0.1) (0.0–0.2) | Private pool | 1 (100) |
| Public pool | 0 (0) | ||
| Sea | 0 (0) | ||
| Unknown | 11 (0.7) (0.3–1.0) | ||
| Other | 5 (0.3) (0.0–0.6) |
We have expressed data on the main mechanisms as absolute frequencies, percentages and 95% confidence intervals (CIs).
Percentages refer to the proportion of the total injuries when it comes to the main mechanisms, and to the proportion of the injuries by that main mechanism when it comes to the subtypes.
Association between mechanism of injury and age group.
| Age | Mechanism of injury | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Fall | Blunt trauma | Athletic activity | Recreational activity | Foreign body | Road traffic accident | Poisoning | Unknown | Other | Total | |
| <1 year | 66 | 5 | 2 | 1 | 2 | 2 | 1 | 1 | 0 | 80 |
| % (95% CI) | 82.5 (74.2–90.8) | 6.3 (0.9–11.6) | 2.5 (0.0–5.9) | 1.3 (0.0–3.7) | 2.5 (0.0–5.9) | 2.5 (0.0–5.9) | 1.3 (0.0–3.7) | 1.3 (0.0–3.7) | ||
| 1–4 years | 240 | 136 | 5 | 27 | 9 | 6 | 16 | 7 | 12 | 458 |
| % (95% CI) | 52.4 (47.8–57.0) | 29.7 (25.5–33-9) | 1.1 (0.1–2.0) | 5.9 (3.7–8.1) | 2.0 (0.7–3.2) | 1.3 (0.3–2.4) | 3.5 (1.8–5.2) | 1.5 (0.4–2.7) | 2.6 (1.2–4.1) | |
| 5–9 years | 210 | 119 | 83 | 82 | 11 | 10 | 2 | 2 | 2 | 521 |
| % (95% CI) | 40.3 (36.1–44.5) | 22.8 (19.2–26.4) | 15.9 (12.8–19.1) | 15.7 (12.6–18.9) | 2.1 (0.9–3.3) | 1.9 (0.7–3.1) | 0.4 (0–0.9) | 0.4 (0–0.9) | 0.4 (0–0.9) | |
| 10–14 years | 186 | 103 | 226 | 58 | 6 | 6 | 1 | 1 | 6 | 593 |
| % (95% CI) | 31.4 (27.6–35.1) | 17.4 (14.3–20.4) | 38.1 (34.2–42.0) | 9.8 (7.4–12.2) | 1.0 (0.2–1.8) | 1.0 (0.2–1.8) | 0.2 (0–0.5) | 0.2 (0–0.5) | 1.0 (0.2–1.8) | |
| 15–16 years | 2 | 3 | 13 | 3 | 0 | 0 | 0 | 0 | 0 | 21 |
| % (95% CI) | 9.5 (0–22.1) | 14.3 (0–29.3) | 61.9 (41.1–82.7) | 14.3 (0–29.3) | ||||||
| Total | 704 | 366 | 329 | 171 | 28 | 24 | 20 | 11 | 20 | 1673 |
| % (95% CI) | 42.1 (39.7–44.4) | 21.9 (19.9–23.9) | 19.7 (17.8–21.6) | 10.2 (8.8–11.7) | 1.7 (1.1–2.3) | 1.4 (0.9–2.0) | 1.2 (0.7–1.7) | 0.7 (0.3–1.0) | 1.2 (0.7–1.7) | 100% |
Data are expressed as absolute frequencies, percentages and 95% confidence intervals (CIs).
Association between the setting of injury and age group.
| Age | Setting of injury | |||||||
|---|---|---|---|---|---|---|---|---|
| Home | School | Child care centre | Street | Sports centre | Playground | Other | Total | |
| <1 year | 63 | 2 | 1 | 7 | 3 | 1 | 3 | 80 |
| % (95% CI) | 78.8 (69.8–87.7) | 2.5 (0–5.9) | 1.3 (0–3.7) | 8.8 (2.6–14.9) | 3.8 (0–7.9) | 1.3 (0–3.7) | 3.8 (0–7.9) | |
| 1–4 years | 243 | 45 | 12 | 75 | 2 | 39 | 42 | 458 |
| % (95% CI) | 53.1 (48.5–57.6) | 9.8 (7.1–12.6) | 2.6 (1.2–4.1) | 16.4 (13.0–19.8) | 0.4 (0–1.0) | 8.5 (6.0–11.1) | 9.2 (6.5–11.8) | |
| 5–9 years | 90 | 161 | 1 | 95 | 44 | 79 | 51 | 521 |
| % (95% CI) | 17.3 (14.0–20.5) | 30.9 (26.9–34.9) | 0.2 (0–0.6) | 18.2 (14.9–21.5) | 8.4 (6.1–10.8) | 15.2 (12.1–18.2) | 9.8 (7.2–12.3) | |
| 10–14 years | 73 | 187 | 0 | 112 | 128 | 56 | 37 | 593 |
| % (95% CI) | 12.3 (9.7–15.0) | 31.5 (27.8–35.3) | 18.9 (15.7–22.0) | 21.6 (18.3–24.9) | 9.4 (7.1–11.8) | 6.2 (4.3–8.2) | ||
| 15–16 years | 2 | 7 | 0 | 3 | 7 | 1 | 1 | 21 |
| % (95% CI) | 9.5 (0–22.1) | 33.3 (13.2–53.5) | 14.3 (0–29.3) | 33.3 (13.2–53.5) | 4.8 (0–13.9) | 4.8 (0–13.9) | ||
| Total | 471 | 402 | 14 | 292 | 184 | 176 | 134 | 1673 |
| % (95% CI) | 28.2 (26.0–30.3) | 24.0 (22.0–26.1) | 0.8 (0.4–1.3) | 17.5 (15.6–19.3) | 11.0 (9.5–12.5) | 10.5 (9.0–12.0) | 8.0 (6.7–9.3) | 100% |
Data are expressed as absolute frequencies, percentages and 95% confidence intervals (CIs).
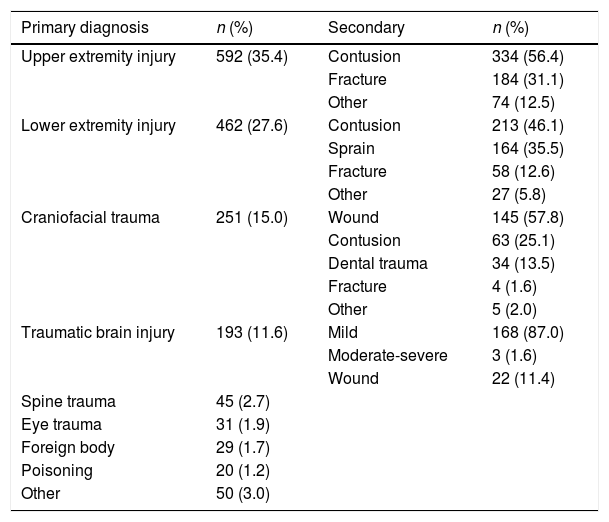
Traumatic injuries amounted to 90% of UIs. They most frequently involved the extremities (Table 5), with 242 fractures in this category (amounting to 14.4% of all UIs and 22.9% of cases of traumatic injury in an extremity).
Diagnoses received by patients with unintentional injuries.
| Primary diagnosis | n (%) | Secondary | n (%) |
|---|---|---|---|
| Upper extremity injury | 592 (35.4) | Contusion | 334 (56.4) |
| Fracture | 184 (31.1) | ||
| Other | 74 (12.5) | ||
| Lower extremity injury | 462 (27.6) | Contusion | 213 (46.1) |
| Sprain | 164 (35.5) | ||
| Fracture | 58 (12.6) | ||
| Other | 27 (5.8) | ||
| Craniofacial trauma | 251 (15.0) | Wound | 145 (57.8) |
| Contusion | 63 (25.1) | ||
| Dental trauma | 34 (13.5) | ||
| Fracture | 4 (1.6) | ||
| Other | 5 (2.0) | ||
| Traumatic brain injury | 193 (11.6) | Mild | 168 (87.0) |
| Moderate-severe | 3 (1.6) | ||
| Wound | 22 (11.4) | ||
| Spine trauma | 45 (2.7) | ||
| Eye trauma | 31 (1.9) | ||
| Foreign body | 29 (1.7) | ||
| Poisoning | 20 (1.2) | ||
| Other | 50 (3.0) |
The percentages of primary diagnoses refer to the proportion over the total of unintentional injuries, and the percentages of secondary diagnoses refer to the proportion over the total for that primary diagnosis.
A total of 34 patients were admitted to hospital (2.0%). The most frequent reason for admission was the need for surgical intervention to set broken bones in the extremities (21; 61.8%). Three children were admitted to the PICU: 1 infant aged 10 months with severe head trauma, 1 infant aged 2 months with a craniofacial fracture due to a fall from a height of more than 1m, and 1 child aged almost 5 years with medication poisoning that required monitoring and administration of activated charcoal). None of the patients died within 24h from the injury.
DiscussionUnintentional injuries are a frequent reason for consultation in Spanish PEDs. The mechanisms involved differ between age groups, although injuries related to falls, blunt trauma and athletic activity amount to 80% of overall visits related to UIs. Although the most frequent diagnosis is contusion of the limb, a fracture was found in more than 20% of cases of trauma to the extremities.
Despite a decline in their incidence in recent years, UIs continue to be the main cause of death in children in the European Union, accounting for 28% of all deaths in children aged 1 to 14 years. The decline is attributed, at least in part, to the impact of child safety programmes implemented in every country of the European Union aimed at preventing potentially fatal accidents (promotion of use of harnessing systems, smoke alarms, fences, window locks, etc.). Nevertheless, visits to emergency departments continue to increase.1 In fact, in our study, nearly 20% of the overall visits to PEDs corresponded to UIs, and while none of the patients died in the first 24h following the event, these injuries caused substantial morbidity. The importance of this problem in our study is consistent with reports from other countries. Thus, it is estimated that 9.2 million children visit emergency departments in the United States due to UIs.9 Taking into account that health professionals employed in PEDs must be prepared to manage any patient seeking emergency care,10 training on the management of patients with UIs should be a priority in the education of paediatricians, with particular emphasis on traumatic injury of the extremities. This is even more important if we consider the high percentage of children that receive outpatient care before arriving to the hospital for this type of traumatic injury.
Several studies have analysed different mechanisms of UI in Spain, such as bicycle accidents, poisonings, road traffic injuries or falls in infants aged less than 1 year.11,12 Our study is the first one to collect comprehensive data on the UIs managed in Spanish PEDs. Its prospective and multicentric design allowed us to obtain information on a large scale with the purpose of identifying opportunities for improvement in the prevention and management of these injuries in Spain. In fact, the design and setting of the study, which allowed us to study the UIs that most worry parents, caregivers and the patients themselves, helped identify epidemiological factors associated with these injuries and compare these findings with other studies. Thus, we found that more than half the patients were injured at home or in school, although the proportion of children injured at home was lower compared to the proportion in the European Injury Database1 and the findings of other studies.13,14 This underscores the need for adequate training not only of parents, but also of the collectives that are commonly in contact with children, such as teachers. We ought to highlight that nearly half of the UIs in our study were not witnessed by an adult, which is consistent with the findings of previous studies, which have shown a frequent lack of supervision of young children and, even more frequently, inadequate adult supervision.11,15 We must emphasise the importance of making adults more aware of the need to closely monitor children and take the necessary precautions, especially at home and in school.
On the other hand, we found a higher frequency of UIs in spring, contrary to a study conducted in primary care that found the peak in autumn, although its authors highlighted the possibility of recall bias in their series.5 These findings may be related to the weather in Spain, which is generally mild. In the United States, for instance, there is a higher incidence of unintentional fractures in the summer.16 In our series, we found a lower frequency of UIs in summer, probably because most of the participating hospitals were in densely populated urban areas, from which families and children are often away during the summer holidays.
We found several incidence peaks involving different mechanisms of injury similar to those found in a study conducted in Spain at the primary care level,5 in which the peak incidence occurred between ages 8 and 11 years, unlike the United States, where the incidence peaks between ages 15 and 19 years.9 However, it is important to remember that not all the PEDs in our study managed patients past the age of 14 years, so that injuries in this age group are probably underrepresented. On the other hand, the percentage of children injured during the weekend was similar to the percentage reported in studies conducted in Spain that analysed falls in infants aged less than 1 year,11 UIs in children managed in primary care5 and UIs in children that required hospital admission.17 This could be due to the weekend being when children spend the most time out of doors, even if it is also the time when they are most likely to be supervised by parents or caregivers.
Falls, and low-energy falls in particular, were the most frequent mechanism of injury overall, as is the case in the European Injury Database1,2 and in the United States.13 This mechanism of injury is particularly important in children aged less than 10 years. However, we must emphasise that there is a broad variety of mechanisms of injury as well as the importance of sports-related injuries in older children.
These patients tended to visit the emergency department early, and a significant number received outpatient care before going to the hospital, especially in the afternoon. Consistently with the existing literature,18 the proportion of children with UIs admitted to hospital was very low and below the proportion of children admitted to hospital for emergencies overall in Spain.
It is particularly alarming that two thirds of children injured in bicycle accidents reported not having worn a helmet, a finding that confirmed the results of a previous multicentre study in Spain.12 It seems obvious that the measures adopted to date are not as effective as expected, despite finding that the percentage of children that were correctly harnessed during road traffic accidents was high.
There are several limitations to our study. On one hand, while it was conducted in 11 hospitals from different regions, it did not include PEDs from every region in Spain, so caution must be exercised in generalising its results to regions that were not included. Also, the hospitals that participated in the study belonged to a research network, although we do not believe that this had an impact on the conclusions of the study, as this is probably not an aspect considered by parents when choosing a facility to seek care for their children. Last of all, the study was conducted in PEDs, which are likely to manage the patients with the most severe or alarming UIs. To develop adequate preventive measures, it is also important to take into account UIs managed in other settings, especially primary care. However, we believe that the information obtained from PEDs is essential to improve these measures.
In conclusion, UIs that occur in different settings account for a significant proportion of the reasons why children seek care in PEDs in Spain. The mechanisms of injury vary based on age. An awareness of the circumstances under which these injuries tend to occur would help develop adequate preventive measures and improve the skills of the individuals in and out of health care that are involved in the management of these children.
Conflicts of interestThe authors have no conflicts of interest to declare.
- -
Cristina Arribas Sánchez, Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
- -
Eduardo J. Bardón Cancho, Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
- -
Arístides Rivas García, Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
- -
Santiago Mintegi, Paediatric Emergency Department, Hospital Universitario de Cruces, Biscay, Spain.
- -
Rafael Marañón Pardillo, Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
- -
Santiago M. Fernández, Paediatric Emergency Department, Hospital Universitario de Cruces, Biscay, Spain.
- -
Anaida Obieta, Paediatric Emergency Department, Hospital Universitario Son Espases, Balearic Islands, Spain.
- -
Nuria Chaves, Paediatric Emergency Department, Hospital Universitario Donostia, Gipuzkoa, Spain
- -
Claudia Farrés, Paediatric Emergency Department, Corporació Sanitària Parc Taulí, Sabadell, Barcelona, Spain.
- -
Gloria Estopiñá, Paediatric Emergency Department, Consorci Sanitari de Terrassa, Terrassa, Barcelona, Spain.
- -
Fernando David Panzino, Paediatric Emergency Department, Hospital General del Parc Sanitari Sant Joan de Déu, Sant Boi de Llobregat, Barcelona, Spain.
- -
Helvia Benito, Paediatric Emergency Department, Hospital Nuestra Señora de Sonsoles, Avila, Spain.
- -
Leticia González, Paediatric Emergency Department, Hospital Universitario Río Hortega, Valladolid, Spain.
- -
María Amalia Pérez, Paediatric Emergency Department, Hospital de Zumárraga, Gipuzkoa, Spain.
- -
Agustín Rodríguez, Paediatric Emergency Department, Hospital Alto Deba, Gipuzkoa, Spain.
Please cite this article as: Arribas Sánchez C, Bardón Cancho EJ, Rivas García A, Mintegi S, Marañón Pardillo R, on behalf of the Observatory group of unintentional injuries of the Research Network of the Spanish Pediatric Emergency Society (RiSeup-Sperg). Consultas relacionadas con lesiones no intencionadas en urgencias en España: serie de casos. An Pediatr (Barc). 2018;89:333–343.
Appendix A lists the names of all the authors of the article.
Previous presentations: This study was presented as a brief communication at the 20th Annual Meeting of the Sociedad Española de Urgencias de Pediatría, April 16–18, 2016, Bilbao, Spain; and as an oral communication at the 21st Annual Meeting of the Sociedad Española de Urgencias de Pediatría, April 14–16, 2016, Valencia, Spain.