The aim of the study was to analyse the evolution, over a 12-year period, of the use of non-invasive (NIV) and invasive ventilation (IV) in children admitted to a paediatric intensive care unit (PICU) due to acute bronchiolitis.
Patients and methodsA retrospective observational study was performed including all children who were admitted to the PICU requiring NIV or IV between 2001 and 2012. Demographic characteristics, ventilation assistance and clinical outcome were analysed. A comparison was made between the first six years and the last 6 years of the study.
ResultsA total of 196 children were included; 30.1% of the subjects required IV and 93.3% required NIV. The median duration of IV was 9.5 days and NIV duration was 3 days. The median PICU length of stay was 7 days, and 2% of the patients died. The use of NIV increased from 79.4% in the first period to 100% in the second period (p<.0001) and IV use decreased from 46% in first period to 22.6% in the last 6 years (p<.0001). Continuous positive airway pressure and nasopharyngeal tube were the most frequently used modality and interface, although the use of bi-level non-invasive ventilation (p<.001) and of nasal cannulas significantly increased (p<.0001) in the second period, and the PICU length of stay was shorter (p=.011).
ConclusionThe increasing use of NIV in bronchiolitis in our PICU during the last 12 years was associated with a decrease in the use of IV and length of stay in the PICU.
Estudiar la evolución durante 12 años del uso de la ventilación mecánica invasiva (VMI) y no invasiva (VNI) en niños con bronquiolitis ingresados en una unidad de cuidados intensivos pediátricos (UCIP).
Pacientes y métodosEstudio retrospectivo observacional de 12 años de duración (2001–2012) en el que se incluyó a todos los niños ingresados con bronquiolitis en UCIP que requirieron VMI y/o VNI. Se analizaron las características demográficas, el tipo de asistencia respiratoria y la evolución clínica, comparándose los primeros 6 años de estudio con los segundos.
ResultadosSe estudió a 196 pacientes. Un 30,1% requirió VMI y un 93,3% VNI. La mediana de duración de VMI fue de 9,5 días y la de VNI de 3 días. La duración de ingreso en UCIP fue de 7 días y falleció un 2% de los pacientes. La utilización de VNI aumentó del 79,4% en el primer periodo al 100% en el segundo periodo (p<0,0001) y disminuyó el de VMI del 46% en el primer periodo al 22,6% en el segundo (p<0,0001). La presión positiva continua en la vía aérea y el tubo endotraqueal cortado fueron la modalidad y la interfase más utilizadas, aunque en el segundo periodo aumentó significativamente el uso de ventilación con 2 niveles de presión (p<0,0001) y de púas nasales (p<0,0001), y disminuyó la duración de ingreso en la UCIP (p=0,011).
ConclusionesLa mayor utilización de VNI en pacientes con bronquiolitis en nuestra unidad en los últimos años se asoció a una disminución de la necesidad de VMI y de la duración del ingreso en la UCIP.
Acute bronchiolitis is the most frequent lower respiratory tract infection in infants and the leading cause of hospital admission in this age group during the epidemic season.
General supportive measures and respiratory support are the mainstay of treatment, as the evidence shows that most pharmacological interventions are not efficacious.1–4
Until a few years ago, a high number of the children with bronchiolitis that developed respiratory failure required invasive mechanical ventilation (IMV), which increased the length of stay and the risk of complications. In recent years, there has been an increase in the use of non-invasive ventilation1 (NIV), but the effects of this treatment on the use of IMV and clinical outcomes are not well understood.
The aim of this study was to analyse the evolution in the use of IMV and NIV in children with acute bronchiolitis admitted to the paediatric intensive care unit (PICU) over a period of 12 years, with the hypothesis that the increase in the use of NIV would be associated with a reduced need for IMV, shorter lengths of stay and lower mortality.
Patients and methodsWe conducted a retrospective observational study of patients admitted to the PICU between January 1, 2001 and December 31, 2012 with a diagnosis of bronchiolitis that required IMV or NIV. Patients that were only treated with high-flow oxygen therapy were not included in the study. We collected data for the following variables: age, sex, need for IMV and NIV, duration of mechanical ventilation, type of NIV: continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP), interface used (nasal cannula, nasopharyngeal endotracheal tube, nasal mask, oronasal mask), mortality, and length of PICU stay. The indication for IMV or NIV was determined by the physician in charge of the patient based on clinical criteria. We performed the statistical analysis with the SPSS 21 software. Our analysis compared two periods of equal length, the first six years of the study (2001–2006) and the last six (2007–2012). We also compared children less and more than 3 months of age. We chose this cut-off point because this is the age threshold for risk reported by other studies. We compared frequencies and medians using the chi square test and Fisher's exact test. The level of statistical significance was set at p<.05.
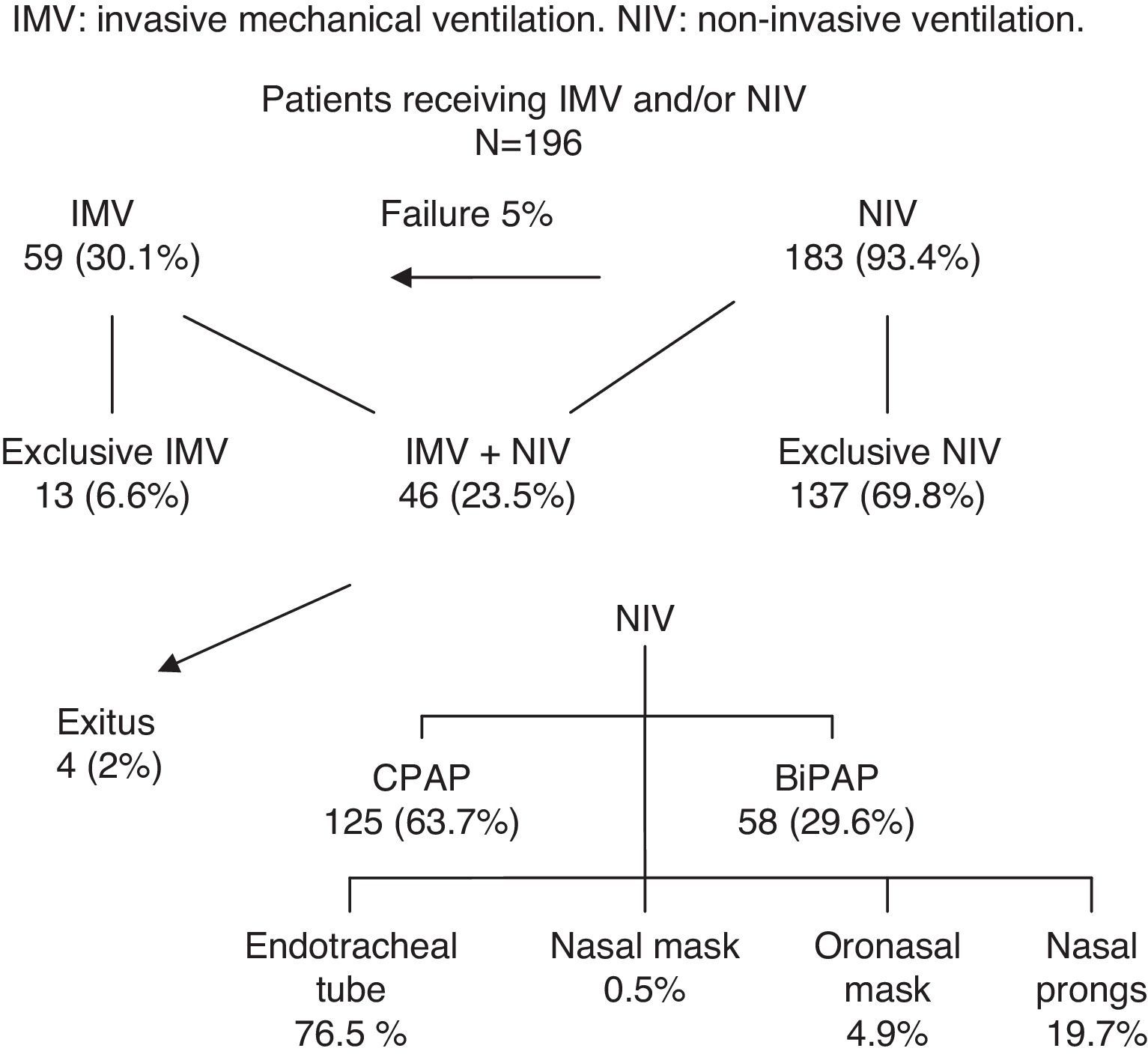
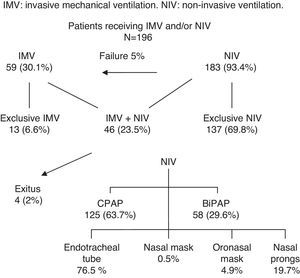
ResultsCharacteristics of patients and mechanical ventilationTable 1 gathers the characteristics of the patients, mechanical ventilation, and outcomes. We analysed the data of 196 patients with a median age of 2 months (interquartile range [IQR], 1–7 months). Of all patients, 57.6% were male. We found risk factors for severe bronchiolitis in 38.3% of the children. Fifty-nine patients (30.1%) required IMV, and 183 (93.4%) required NIV. Among the patients, 69.9% only required NIV, 6.6% required only IMV, and 23.5% were treated with both. The most frequently used mode of NIV was CPAP (68.3%) and the most frequently used interface was the nasopharyngeal tube (76.5%).
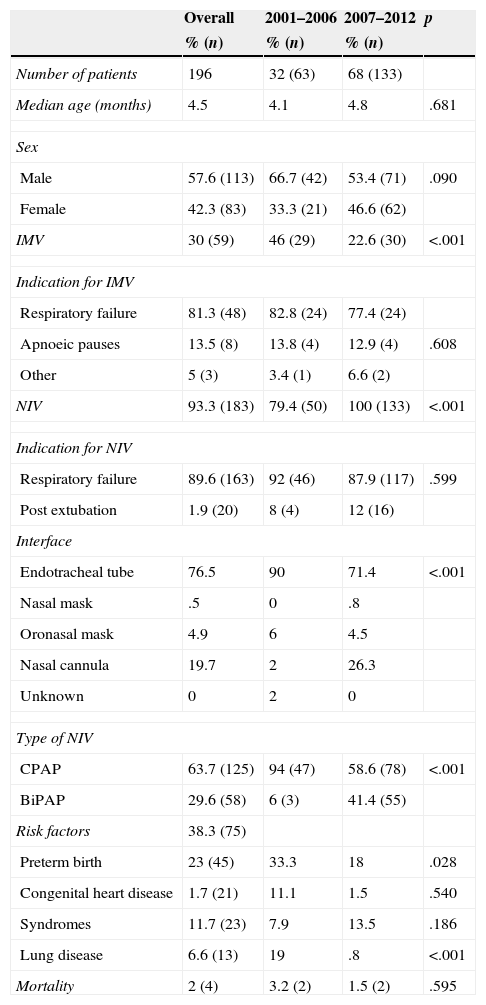
Demographic characteristics, respiratory support and mortality. Comparison of the two periods under study.
| Overall | 2001–2006 | 2007–2012 | p | |
|---|---|---|---|---|
| % (n) | % (n) | % (n) | ||
| Number of patients | 196 | 32 (63) | 68 (133) | |
| Median age (months) | 4.5 | 4.1 | 4.8 | .681 |
| Sex | ||||
| Male | 57.6 (113) | 66.7 (42) | 53.4 (71) | .090 |
| Female | 42.3 (83) | 33.3 (21) | 46.6 (62) | |
| IMV | 30 (59) | 46 (29) | 22.6 (30) | <.001 |
| Indication for IMV | ||||
| Respiratory failure | 81.3 (48) | 82.8 (24) | 77.4 (24) | |
| Apnoeic pauses | 13.5 (8) | 13.8 (4) | 12.9 (4) | .608 |
| Other | 5 (3) | 3.4 (1) | 6.6 (2) | |
| NIV | 93.3 (183) | 79.4 (50) | 100 (133) | <.001 |
| Indication for NIV | ||||
| Respiratory failure | 89.6 (163) | 92 (46) | 87.9 (117) | .599 |
| Post extubation | 1.9 (20) | 8 (4) | 12 (16) | |
| Interface | ||||
| Endotracheal tube | 76.5 | 90 | 71.4 | <.001 |
| Nasal mask | .5 | 0 | .8 | |
| Oronasal mask | 4.9 | 6 | 4.5 | |
| Nasal cannula | 19.7 | 2 | 26.3 | |
| Unknown | 0 | 2 | 0 | |
| Type of NIV | ||||
| CPAP | 63.7 (125) | 94 (47) | 58.6 (78) | <.001 |
| BiPAP | 29.6 (58) | 6 (3) | 41.4 (55) | |
| Risk factors | 38.3 (75) | |||
| Preterm birth | 23 (45) | 33.3 | 18 | .028 |
| Congenital heart disease | 1.7 (21) | 11.1 | 1.5 | .540 |
| Syndromes | 11.7 (23) | 7.9 | 13.5 | .186 |
| Lung disease | 6.6 (13) | 19 | .8 | <.001 |
| Mortality | 2 (4) | 3.2 (2) | 1.5 (2) | .595 |
BiPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; IMV, invasive mechanical ventilation; NIV, non-invasive ventilation.
The median duration of IMV was 9.5 days (IQR 6–14 days) and that of NIV was 3 days (IQR, 1–4 days). Intubation was required after failure of NIV in 5.1% of children. Patients treated with CPAP required intubation less frequently (2.4%) than patients treated with BiPAP (10.3%) (p=.030) and patients that received ventilation support through an endotracheal tube (2.9%) less frequently than through the other interfaces (11.6%) (p=.034). The median length of PICU stay was 7 days (IQR, 4–14 days). Four patients (2%) died of respiratory failure refractory to treatment and severe pulmonary hypertension. All four had been treated with NIV, IMV and high-frequency ventilation and three had undergone extracorporeal membrane oxygenation. Patient outcomes are presented in Fig. 1.
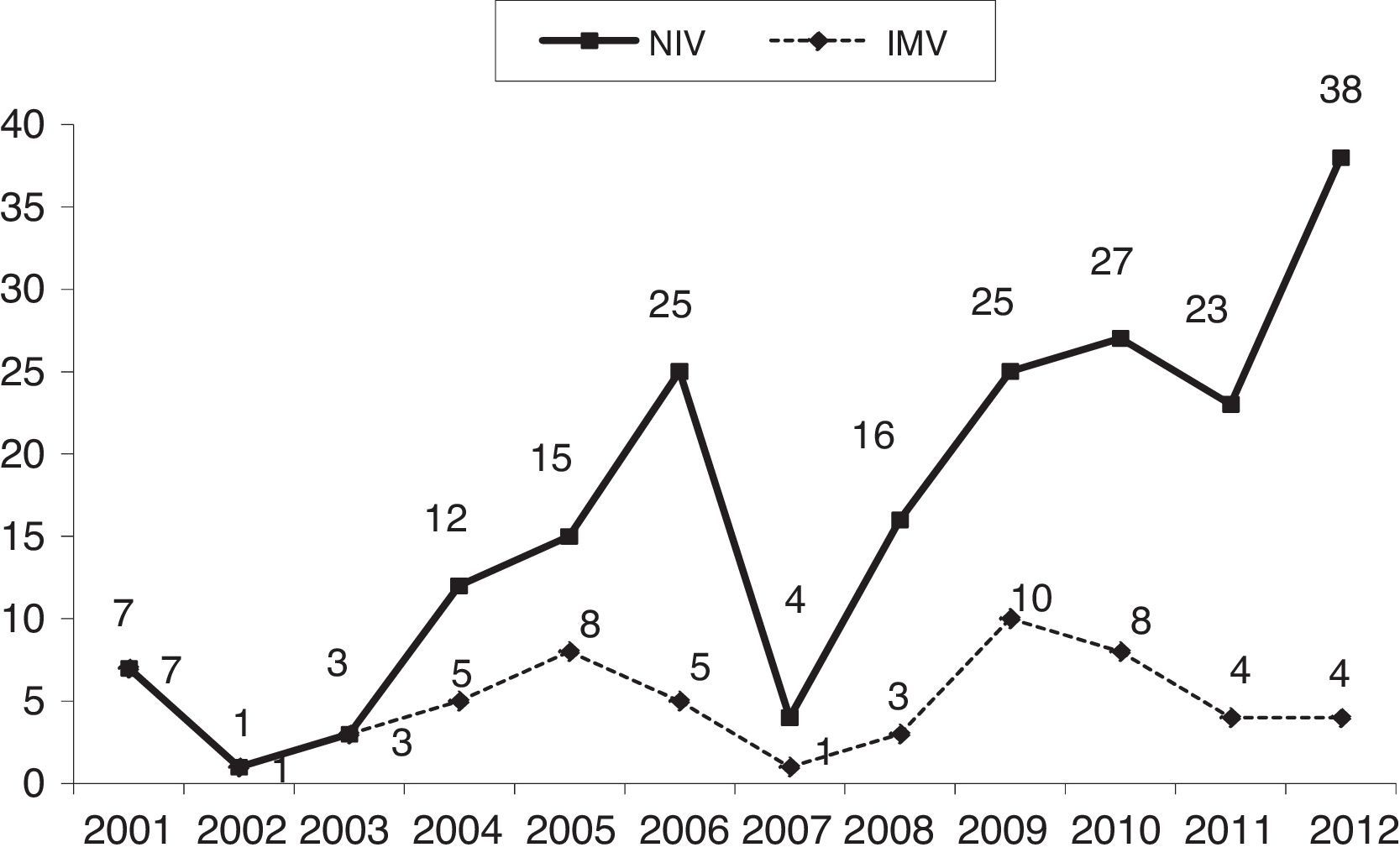
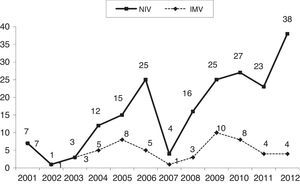
Comparison of the two periods under studyTable 1 compares the characteristics of the first and second six-year periods. The number of patients admitted for bronchiolitis increased significantly in the second period. The incidence of preterm birth and chronic pulmonary disease was higher in the first six years under study compared to the last six. There were no differences in age or sex between the two periods. The use of NIV was significantly greater in the second period, and increased as years passed (Fig. 2). Fewer patients needed IMV in the second period, and there were no differences in the indications for IMV or NIV. The use of BiPAP and of nasal cannulae increased significantly in the second period. There were no differences in duration of IMV, with a median of 10 days (IQR, 4.5–16.5) in the first period compared to 9 days (IQR, 6–14) in the second (p=.906), or in the duration of NIV, which was of 3 days (IQR, 1–4.7) in the first period compared to 3 days (IQR, 1.2–4) in the second (p=.547). The length of PICU stay was longer in the first period (9 days; IQR, 5–17) than in the second (6 days; IQR, 4–12) (p=.040).
The overall mortality was 2% (4 patients), with two patients dying in the first period and another two in the second and no significant differences between periods, although mortality in relation to the number of admissions was slightly lower in the second period (3.2% of admissions in the first period versus 1.5% in the second) (Table 1).
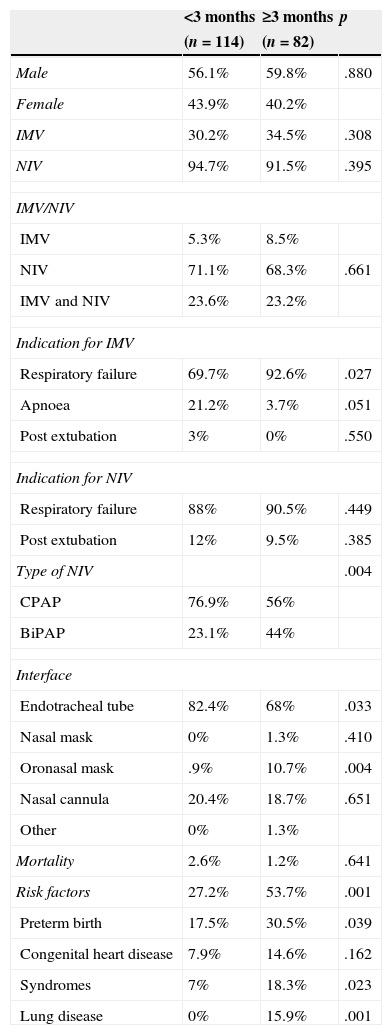
Comparison by ageTable 2 compares children older and younger than 3 months. Endotracheal tubes and CPAP were used more often in children younger than 3 months, and oronasal masks in older children. Apnoeic pauses were the most frequent indication for NIV in children younger than 3 months (p=.051) while the leading indication in older children was respiratory failure (p=.027).
Comparison by age group.
| <3 months | ≥3 months | p | |
|---|---|---|---|
| (n=114) | (n=82) | ||
| Male | 56.1% | 59.8% | .880 |
| Female | 43.9% | 40.2% | |
| IMV | 30.2% | 34.5% | .308 |
| NIV | 94.7% | 91.5% | .395 |
| IMV/NIV | |||
| IMV | 5.3% | 8.5% | |
| NIV | 71.1% | 68.3% | .661 |
| IMV and NIV | 23.6% | 23.2% | |
| Indication for IMV | |||
| Respiratory failure | 69.7% | 92.6% | .027 |
| Apnoea | 21.2% | 3.7% | .051 |
| Post extubation | 3% | 0% | .550 |
| Indication for NIV | |||
| Respiratory failure | 88% | 90.5% | .449 |
| Post extubation | 12% | 9.5% | .385 |
| Type of NIV | .004 | ||
| CPAP | 76.9% | 56% | |
| BiPAP | 23.1% | 44% | |
| Interface | |||
| Endotracheal tube | 82.4% | 68% | .033 |
| Nasal mask | 0% | 1.3% | .410 |
| Oronasal mask | .9% | 10.7% | .004 |
| Nasal cannula | 20.4% | 18.7% | .651 |
| Other | 0% | 1.3% | |
| Mortality | 2.6% | 1.2% | .641 |
| Risk factors | 27.2% | 53.7% | .001 |
| Preterm birth | 17.5% | 30.5% | .039 |
| Congenital heart disease | 7.9% | 14.6% | .162 |
| Syndromes | 7% | 18.3% | .023 |
| Lung disease | 0% | 15.9% | .001 |
BiPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; IMV, invasive mechanical ventilation; NIV, non-invasive ventilation.
More than one interface was used in some patients.
There were no differences in the duration of IMV, with a median of 10 days (IQR, 7–14.2) in children younger than 3 months compared to 8.5 days (IQR, 4.5–15) in older children (p=.415); the duration of NIV, with a median of 3 days (IQR, 1–4) in infants younger than 3 months compared to 2 days (IQR, 1–4.2) in older patients (p=.631); or the length of stay in the PICU, which was of 7 days (IQR, 4–15) in patients younger than 3 months compared to 7 days (IQR, 4–11.5) in older ones (p=.495). While we found no significant differences in mortality between both groups, it was slightly higher in patients younger than 3 months (Table 2).
Comparison by indication for ventilationPatients that required IMV had a higher mortality (8.7%) than those that required NIV alone (0%) (p<.001) and had a longer length of stay (9 days; IQR, 6–16.5) than those treated with NIV only (5 days; IQR, 4–8.5) (p<.001). Children that required both types of ventilation (IMV and NIV) had longer lengths of stay (17 days; IQR, 11–25.25) than children who were treated with IMV or NIV alone (p<.001). The length of stay was longer in children treated with NIV following extubation (19.5 days; IQR, 14–31) compared to children that required NIV due to initial respiratory failure (6 days; IQR, 4–10) (p<.001). The duration of NIV in children in whom it was indicated post extubation was of 4.9 days (IQR 1–4), while it was 3.1 days (IQR, 1–4) in children in whom it was indicated due to respiratory failure (p<.001). Patients treated with BiPAP had longer lengths of stay (15.4 days; IQR, 5–21) compared to those treated with CPAP (9.3; IQR, 4–13) (p=.002). The duration of NIV in patients treated with BiPAP was of 4 days (IQR, 1–4.5), while it was of 2 days (IQR, 1–4) in children treated with CPAP (p=.022).
DiscussionClassic therapeutic measures indicated for bronchiolitis, such as aerosol therapy, humidity and physical therapy, have demonstrated poor effectiveness in the management of respiratory failure secondary to this illness.1–4
In recent years, NIV and high-flow oxygen therapy have gained importance in the management of children with bronchiolitis, and several studies have analysed its effects.5–18 Our study is the one that has analysed the outcomes of NIV characteristics (interfaces and modes) for the longest period of time, which allowed us to assess their effects on length of stay and need for IMV.
Our study found a significant increase in the number of PICU admissions for bronchiolitis in recent years1,19,20 as well as a more frequent use of NIV. This increase in NIV use was accompanied by a reduced need for IMV, consistent with other studies,3,7,21–23 and by a shorter length of stay in the PICU. These findings are highly significant and evince an important advance in treatment, as this can lead to decreased mortality and contribute to cost reduction, although our study did not analyse these variables.
In the second period under study, the percentage of patients with risk factors was significantly lower than in the first period. This may suggest that the severity of disease was greater in patients in the first period compared to patients in the second period, or that the indications for admission and treatment with NIV were different in both periods, with NIV being initiated earlier in recent years. Thus, we cannot rule out a bias in the indication for NIV, as our study did not analyse the degree of severity of respiratory failure prior to treatment with NIV. However, the reason for admission to the PICU and for using NIV was failure of other measures of respiratory support, and in the last period of the study many of the patients had been treated with high-flow oxygen in the hospital ward.
Patients treated with IMV had longer lengths of stay than patients that required NIV alone, results that are similar to those found in other studies.23 The duration of IMV was longer in the first period under study, and duration of NIV was longer in the second, although these differences did not reach statistical significance. These findings suggest that the use of NIV reduces the need for IMV and lengths of stay. However, given that we conducted a long-term retrospective study and that we did not assess the degree of severity of respiratory failure, we cannot rule out the influence of other factors in these findings.
The types of interface used in NIV changed throughout the study, with a progressive increase in the use of bilevel pressure modes that offer more support to the patient, and of nasal cannulae as an interface, which while offering less respiratory support are better tolerated by the patient. Consequently, nasal and oronasal masks have come to be used only in patients with more severe respiratory failure or when treatment with other interfaces fails. Other interfaces, such as helmets and full-face masks, were not used in this study.
Our results show that patients that receive NIV post extubation have longer lengths of stay in the PICU, which makes sense considering that they had previously required IMV, and thus had had more severe respiratory insufficiency. The length of stay was also longer in children treated with BiPAP. This is not to say that BiPAP is less effective than CPAP, and may be due to the bilevel pressure mode being used in children with more severe respiratory failure.
In children younger than 3 months, CPAP was the most frequently used type of NIV and endotracheal tubes were the most frequently used interface. This is because there are still few bilevel (BiPAP) NIV interfaces that adapt well to the smallest infants, and because these patients tolerate a shortened endotracheal tube placed in the nasopharynx through a nostril better than other children.24
In our study, contrary to what happened in others,1,2,16 patients younger than 3 months did not require IMV more frequently nor had higher lengths of stay or mortality. Our results show that NIV may be useful in children with bronchiolitis irrespective of their age. However, we must interpret these results with caution, as we cannot rule out the presence of a severity bias. Thus, large-scale prospective studies are required to confirm these findings.
We found a percentage of NIV failure that was lower than those described in other studies.2–4 This could be due to earlier initiation of NIV in patients with milder degrees of respiratory failure, but we could not confirm this hypothesis, as respiratory failure characteristics were not documented at the time NIV was initiated.
There are several limitations to our study. First, we did not compare patients receiving NIV with a control group. We believe that such a study would not be ethically justified at the moment. The most important limitation is that this was a retrospective study in which we could not document the severity of respiratory failure, which, as we mentioned, may influence our results. We were also unable to assess the effect of the NIV mode and interface used in each patient. Thus, prospective studies ought to be conducted that analyse the relationship between the severity of respiratory failure, NIV characteristics, and interface type used on the need for IMV and the length of stay in the PICU.
We have concluded that bronchiolitis is the cause of a considerable number of PICU admissions. In our experience, the increased use of NIV is associated with a reduced need for IMV and a shorter length of stay in the PICU.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: del Castillo BT, Lafever SNF, Sanguos CL, Sánchez LD-C, da Silva MS, Cid JL-H. Evolución de la ventilación mecánica no invasiva en la bronquiolitis. An Pediatr (Barc). 2015;83:117–122.