Kawasaki disease (KD) is an acute vasculitis of unknown origin and predominant in males. The long-term effects of the disease depend on whether there are coronary lesions, particularly aneurysms. The prognosis of patients with giant aneurysms is very poor due to their natural progression to coronary thrombosis or severe obstructive lesions.
ObjectivesA series of 8 cases is presented where the epidemiology and diagnostic methods are described. The treatment of the acute and long-term cardiovascular sequelae is also reviewed.
MethodsA descriptive analysis was conducted on patients admitted to the Paediatric Cardiology Unit of La Fe University Hospital (Valencia) with KD and a coronary lesion.
ResultsMore than one artery was involved in all patients. Although early diagnosis was established in only two cases, none of the patients had severe impairment of ventricular function during the acute phase. Treatment included intravenous gammaglobulin and acetylsalicylic acid at anti-inflammatory doses during the acute phase. A combination of dual antiplatelet therapy and corticosteroids was given in cases of coronary thrombosis. The silent aneurysms continue to persist.
ConclusionsKD is the most common cause of acquired heart disease in children. The delay in diagnosis is associated with a greater likelihood of coronary lesions that could increase the risk of cardiovascular events in adulthood. Thus, this subgroup requires close clinical monitoring for a better control of cardiovascular risk factors over time.
La enfermedad de Kawasaki (EK) es una vasculitis aguda de causa desconocida, predominante en el sexo masculino. Los efectos de la enfermedad a largo plazo dependen de la existencia de lesiones coronarias —aneurismas—, siendo el pronóstico de los pacientes con aneurismas gigantes sombrío, ya que en su evolución natural pueden presentar trombosis coronaria o lesiones obstructivas severas.
ObjetivosDescribimos las características de una serie de 8 pacientes lactantes con EK y severa afectación coronaria. Se describen la epidemiología y los métodos diagnósticos, y se revisa el tratamiento de la fase aguda, así como las secuelas cardiovasculares a largo plazo.
MétodosSe realizó un análisis descriptivo de pacientes ingresados en el Servicio de Cardiología Pediátrica del Hospital Universitario La Fe (Valencia) por EK con afectación coronaria.
ResultadosEn todos los casos se objetivó la afectación de más de una arteria. El diagnóstico se instauró precozmente en solo 2 casos, a pesar de ello, ningún paciente presentó deterioro grave de la función ventricular durante la fase aguda. El tratamiento incluyó gammaglobulina por vía intravenosa y ácido acetilsalicílico en dosis antiinflamatorias durante la fase aguda. En los casos de trombosis coronaria se asociaron doble antiagregación y corticoides. Las lesiones aneurismáticas silentes persisten hasta el momento actual.
ConclusionesLa EK es la causa más común de enfermedad cardiaca adquirida en niños. El retraso en el diagnóstico se asocia a mayor frecuencia de lesiones coronarias, que podrían incrementar el riesgo de eventos cardiovasculares en la edad adulta, precisando este subgrupo un seguimiento clínico estrecho con control de los factores de riesgo cardiovascular a largo plazo.
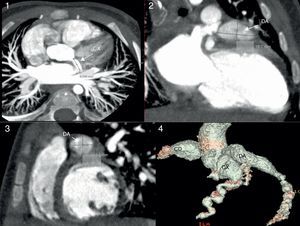
Kawasaki disease (KD) is one of the most frequent vasculitis in children, and its aetiology remains unknown. It is more prevalent in children of Asian descent and aged 2–5 years.1,2 Any of the structures of the heart may be affected, but coronary involvement is the most feared complication, as formation of coronary aneurysms (CAs) may result in thrombosis, ischaemic heart disease, early-onset atherosclerosis and sudden death, especially aneurysms of large size, which are associated with more frequent complications (stenosis/thrombosis). Treatment during the acute phase aims at controlling the systemic inflammatory state, while the long-term objective is to prevent ischaemic heart disease in patients that develop coronary lesions3 (Figs. 1–4).
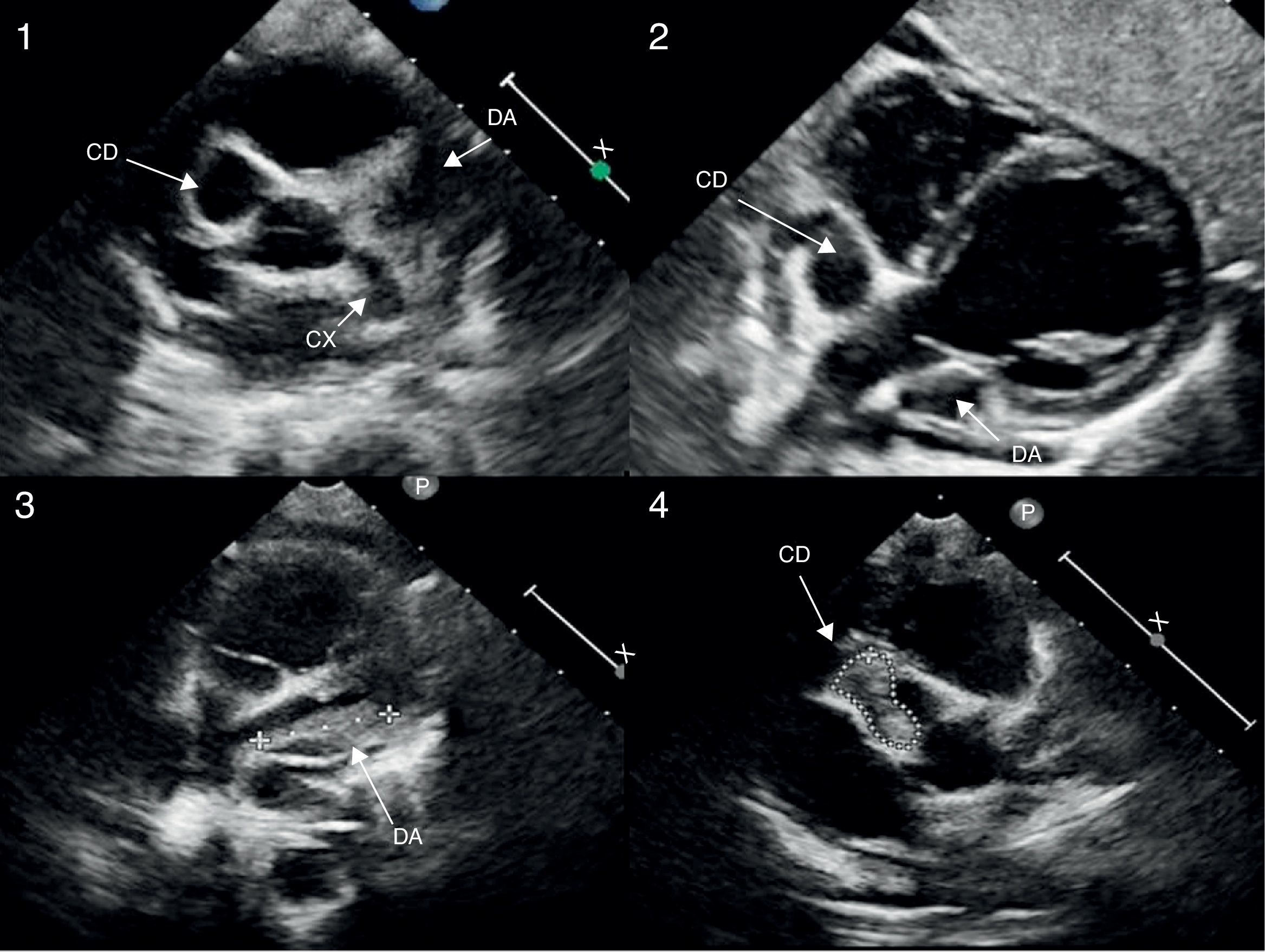
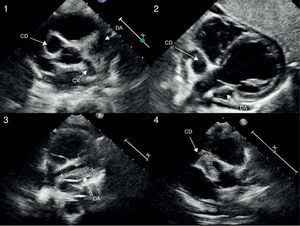
Echocardiogram (modified high parasternal short-axis view at the level of the large arteries for assessment of aortic arch and coronary arteries) revealing the presence of giant aneurysms in the proximal segments of the three major coronary arteries (images 1 and 2). Follow-up echocardiogram showing intraluminal thrombi in the LAD and RCA, with preserved systolic function (images 3 and 4).
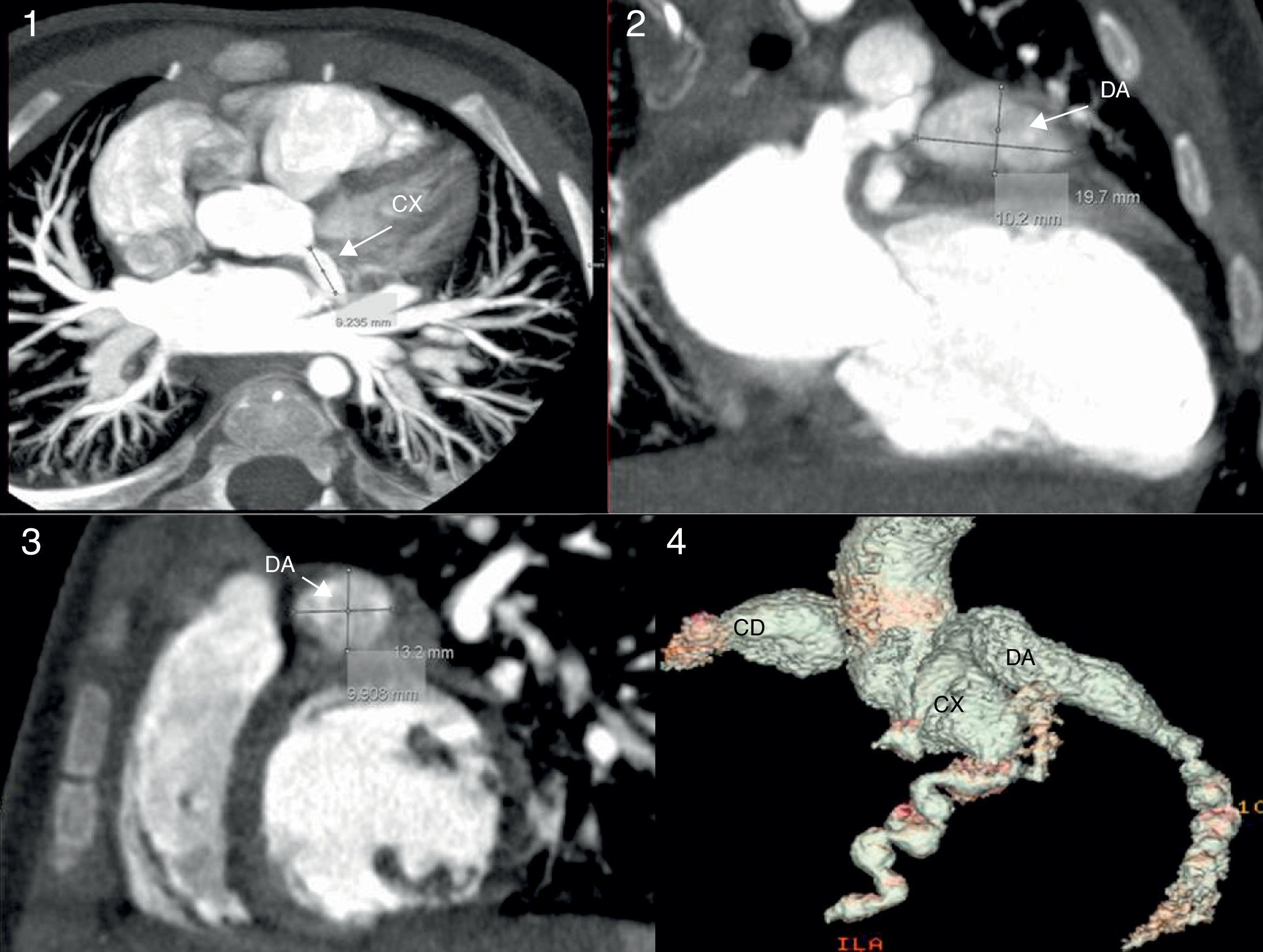
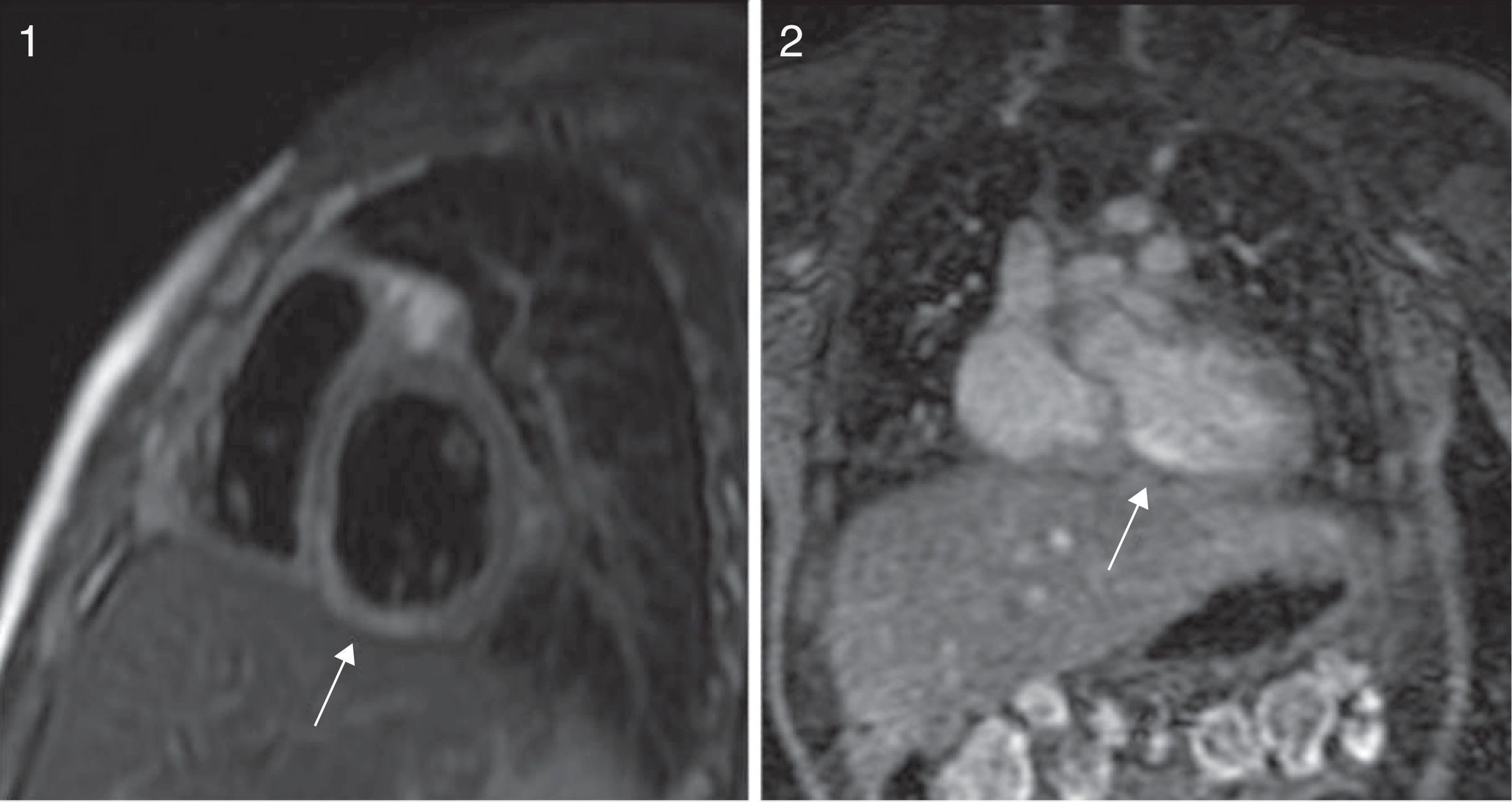
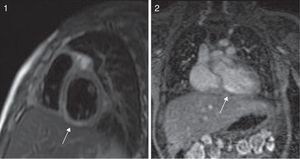
Cardiac CT scan. The proximal giant-sized aneurysmal dilatation in the LAD and RCA can be seen in the three views of the multiplanar reconstruction: axial (image 1), coronal (image 2), and sagittal (image 3); the 3D reconstruction (image 4) accurately shows the location, extension and size of the aneurysms. Localisation of hypoperfusion in the inferior wall, necrosis and lack of viability in one segment (image 1) and hypoperfusion without signs of myocardial injury in the LAD region (image 2).
We conducted a retrospective descriptive analysis between October 2004 and May 2015. We included 8 patients aged less than 2 years that met the criteria for complete or incomplete KD (Table 1) and giant CAs.
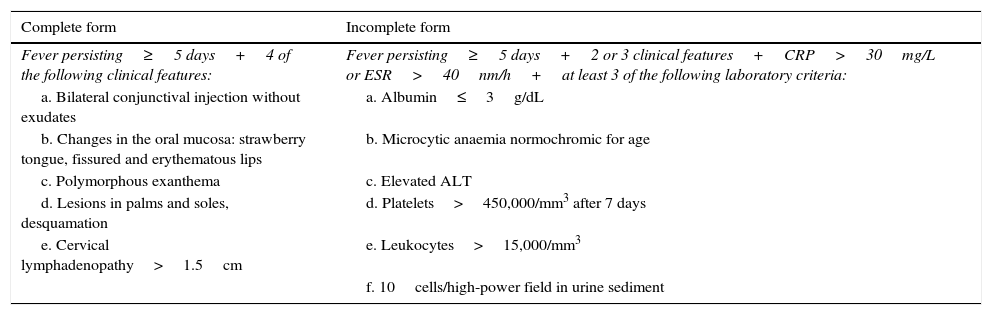
Diagnostic criteria for Kawasaki disease.
| Complete form | Incomplete form |
|---|---|
| Fever persisting≥5 days+4 of the following clinical features: | Fever persisting≥5 days+2 or 3 clinical features+CRP>30mg/L or ESR>40nm/h+at least 3 of the following laboratory criteria: |
| a. Bilateral conjunctival injection without exudates | a. Albumin≤3g/dL |
| b. Changes in the oral mucosa: strawberry tongue, fissured and erythematous lips | b. Microcytic anaemia normochromic for age |
| c. Polymorphous exanthema | c. Elevated ALT |
| d. Lesions in palms and soles, desquamation | d. Platelets>450,000/mm3 after 7 days |
| e. Cervical lymphadenopathy>1.5cm | e. Leukocytes>15,000/mm3 |
| f. 10cells/high-power field in urine sediment |
Adapted from the Japanese Ministry of Health Research Committee and the American Heart Academy of Pediatrics.
Based on the description by Kawasaki in 1967, Kawasaki disease is defined as the presence of fever persisting more than 5 days with at least four of the following criteria: bilateral conjunctival injection without exudate, oral changes (strawberry tongue), erythema and desquamation in hands and feet, polymorphous nonpetechial rash and adenopathies (Table 1).4 Incomplete KD is diagnosed if only 2 or 3 of the 5 criteria are met. When it comes to laboratory criteria, KD is invariably associated with an inflammatory process, with increases in erythrocyte sedimentation rates (ESR>20mmHg), C-reactive protein levels (CRP>30mg/L) and white blood cell counts (>12,000/mm3). Thrombocytosis (platelets>450,000/mm3) develops late in the second week from onset, and thus has no diagnostic value during the acute phase, when the platelet count may be low or normal (poorer prognosis). Other changes in laboratory parameters include hyperbilirubinaemia, hypertransaminasemia, hypoalbuminaemia (<3.5g/dL), sterile pyuria and cerebrospinal fluid pleocytosis.
On admission to our hospital, patients with suspected KD underwent a cardiovascular assessment that included a full physical examination, electrocardiography and echocardiography. Coronary changes were classified as ectasias, small aneurysms (<5mm), medium-sized aneurysms (5–6mm), giant aneurysms (>6–8mm and/or z-score≥10),5,6 and coronary stenosis/thrombosis. In cases with extensive coronary involvement, performance of a coronary CT angiography (CCTA) is currently recommended to characterise anatomical abnormalities and detect complications. Furthermore, the development of magnetic resonance imaging (MRI) and its application to the measurement of myocardial perfusion with the administration of intravenous dipyridamole (IVDP) allows a more detailed assessment of myocardial injury and the viability of the damaged tissue.
We collected data for the following variables: sex, age, season of year, duration of fever in days, clinical and laboratory criteria (including brain natriuretic peptide [pro-BNP] or myocardial injury markers [troponin T]), imaging tests such as echocardiography, computed tomography (CT) and other functional imaging techniques like myocardial perfusion imaging or MRI with IVDP, and the treatment received.
As for the treatments used and their dosages, intravenous immunoglobulin therapy (IVIG) was administered through continuous infusion over 12h in doses of 2g/kg/dose, acetylsalicylic acid (ASA) was used during the acute phase at anti-inflammatory doses (80–100mg/kg/day) and decreased to antiplatelet doses (3–5mg/kg/day) once the fever had resolved. Nonresponse to treatment was defined as persistence of fever for more than 36h after administration of IVIG. Two different regimens were used for steroids (patients were not contemporary); the earliest patients received IV prednisone at doses of 1–2mg/kg/day for 5–7 days, and recent patients received IV methylprednisolone at doses of 30mg/kg/day for 3 days. In patients with coronary involvement in whom adequate anticoagulation could not be achieved and clinical and laboratory features of persisting and uncontrolled inflammation, infliximab (5mg/kg in a single IV dose), a monoclonal antibody with potent anti-inflammatory properties, was used for rescue anti-inflammatory treatment.
The first-line anticoagulant therapy consisted of low-molecular-weight heparin (enoxaparin) at a dose of 1mg/kg/day administered subcutaneously, although heparin sodium administered by continuous infusion at doses of 28IU/kg/h was preferred in cases with coronary thrombosis. Abciximab (a monoclonal antibody that blocks the cascade that generates thrombin following platelet activation) was used in patients with coronary thrombosis in combination with ASA and heparin sodium and administered by continuous infusion at doses of 1.5IU/kg/h (0.25μg/kg/min) over 12h. Tissue plasminogen activator (TPA) is an enzyme involved in the breakdown of blood clots (it catalyses the conversion of plasminogen to plasmin, which is the main enzyme involved in clot dissolution); recombinant TPA (r-TPA) was used at low doses (0.1mg/kg/h) due to the young age of the patients, and administered by continuous infusion over 12h. The prophylactic antithrombotic treatment prescribed at discharge consisted of ASA and acenocoumarol to maintain the international normalised ratio (INR) in the 2-to-2.5 range.
ResultsThe age of the 8 patients in our series ranged between 5 and 24 months, with a majority of infants (median age, 8.3 months) and boys (62.5%). Ninety percent of patients had onset during the cold seasons (winter, autumn). When it came to diagnosis, which was based on classic clinical criteria from 1974 reviewed by Jane et al. in 2004,2 all of the patients presented with persistent fever, with a temperature of more than 39°C in 90% of them. All patients presented with polymorphous exanthema; mucosal inflammation and bilateral conjunctivitis without exudate were found in 50%, and cervical adenitis was only found in one of the latter group, so that most cases (6 patients) were initially diagnosed as incomplete KD (Table 1). Three out of the 8 patients had a different initial diagnosis (1 of viral infection, 1 of bacteraemia and 1 of liver failure and encephalitis in the context of sepsis) and only 2 patients (cases 6 and 8) met the criteria for complete KD.
As for the changes in laboratory parameters at the time of diagnosis (understood as the time of prescription of specific immunoglobulin infusion therapy), leukocytosis was found in all cases, and 6 out of 8 patients (75%) presented with marked thrombocytosis (the other 2 cases were diagnosed at earlier stages). All patients had changes in the levels of acute phase reactants, with elevation of CRP in all eight and increased ESRs in seven. In our series, all patients presented with hypoalbuminaemia at the time of diagnosis. There was a significant increase in the levels of myocardial injury markers and pro-BNP in all patients, with a mild elevation of troponin T and pro-BNP overall and very high levels in the 2 patients (25%) with coronary thrombosis (troponin T>2ng/mL; pro-BNP>15,000pg/mL). None of the patients experienced severe heart failure.
In most patients, coronary abnormalities were first detected by Doppler echocardiography in most patients (Fig. 1), except in one patient (case 4) in whom viral illness was initially suspected and the first diagnostic test was a chest CT scan requested due to the presence of infiltrates in both upper lobes that detected coronary abnormalities, which were later confirmed by echocardiography. In all cases, imaging detected abnormalities in more than one artery.
In regards to treatment, it was initiated quickly in the 2 patients that met the classic diagnostic criteria (Table 2) on arrival to the reference hospital (cases 6 and 8); in the rest of patients, targeted treatment was not initiated that early because KD was not suspected at the beginning. Treatment in all patients was initiated with IVIG and ASA, the latter at anti-inflammatory doses during the acute-subacute phase until inflammatory marker levels descended and patients had been afebrile for a sustained period of time, and then continued with antiplatelet doses after discharge. The median number of days of fever during which immunoglobulin therapy was administered was 12.25 (minimum, 9 days; maximum, 23 days). Five patients required repeated doses of IVIG due to a lack of clinical response, which led to the additional prescription of steroids (3 of them received the original prednisone regimen, and 2 of them, at a later time, the methylprednisolone regimen); 2 of them (the patients with intracoronary thrombosis) also received unit doses of infliximab.
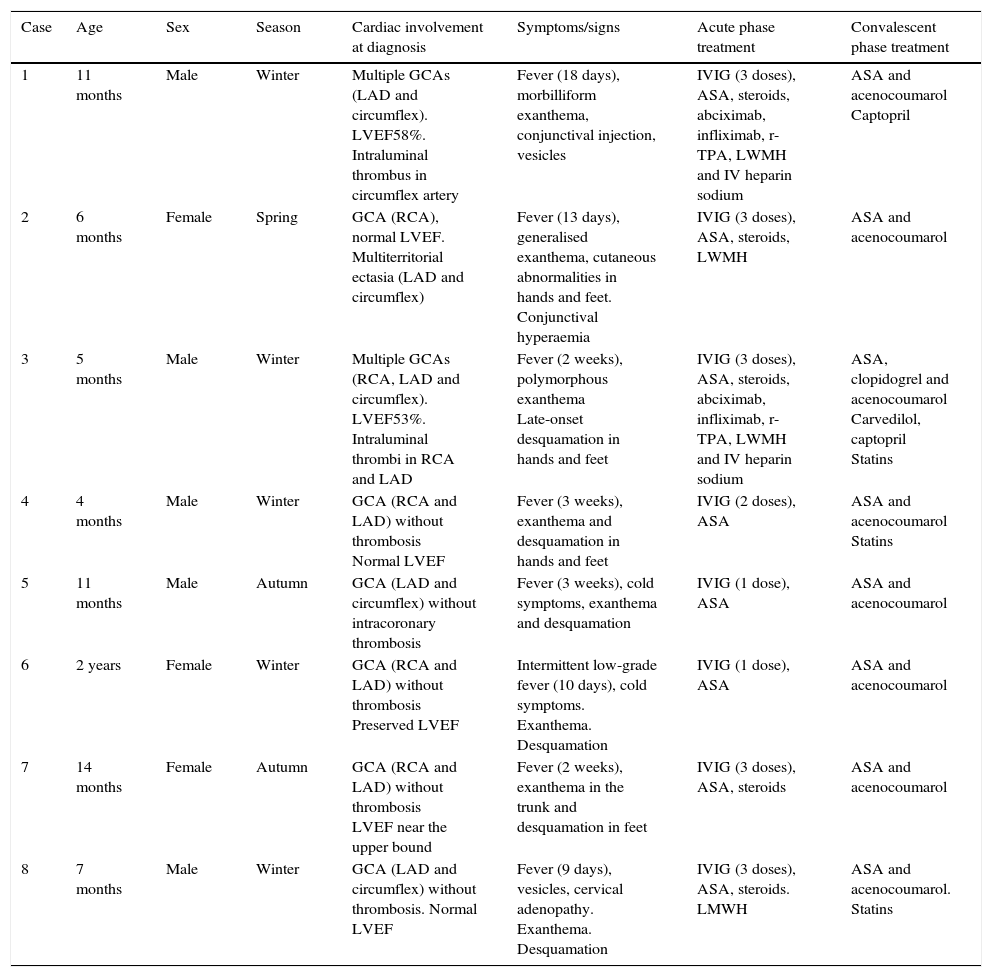
Sample characteristics.
| Case | Age | Sex | Season | Cardiac involvement at diagnosis | Symptoms/signs | Acute phase treatment | Convalescent phase treatment |
|---|---|---|---|---|---|---|---|
| 1 | 11 months | Male | Winter | Multiple GCAs (LAD and circumflex). LVEF58%. Intraluminal thrombus in circumflex artery | Fever (18 days), morbilliform exanthema, conjunctival injection, vesicles | IVIG (3 doses), ASA, steroids, abciximab, infliximab, r-TPA, LWMH and IV heparin sodium | ASA and acenocoumarol Captopril |
| 2 | 6 months | Female | Spring | GCA (RCA), normal LVEF. Multiterritorial ectasia (LAD and circumflex) | Fever (13 days), generalised exanthema, cutaneous abnormalities in hands and feet. Conjunctival hyperaemia | IVIG (3 doses), ASA, steroids, LWMH | ASA and acenocoumarol |
| 3 | 5 months | Male | Winter | Multiple GCAs (RCA, LAD and circumflex). LVEF53%. Intraluminal thrombi in RCA and LAD | Fever (2 weeks), polymorphous exanthema Late-onset desquamation in hands and feet | IVIG (3 doses), ASA, steroids, abciximab, infliximab, r-TPA, LWMH and IV heparin sodium | ASA, clopidogrel and acenocoumarol Carvedilol, captopril Statins |
| 4 | 4 months | Male | Winter | GCA (RCA and LAD) without thrombosis Normal LVEF | Fever (3 weeks), exanthema and desquamation in hands and feet | IVIG (2 doses), ASA | ASA and acenocoumarol Statins |
| 5 | 11 months | Male | Autumn | GCA (LAD and circumflex) without intracoronary thrombosis | Fever (3 weeks), cold symptoms, exanthema and desquamation | IVIG (1 dose), ASA | ASA and acenocoumarol |
| 6 | 2 years | Female | Winter | GCA (RCA and LAD) without thrombosis Preserved LVEF | Intermittent low-grade fever (10 days), cold symptoms. Exanthema. Desquamation | IVIG (1 dose), ASA | ASA and acenocoumarol |
| 7 | 14 months | Female | Autumn | GCA (RCA and LAD) without thrombosis LVEF near the upper bound | Fever (2 weeks), exanthema in the trunk and desquamation in feet | IVIG (3 doses), ASA, steroids | ASA and acenocoumarol |
| 8 | 7 months | Male | Winter | GCA (LAD and circumflex) without thrombosis. Normal LVEF | Fever (9 days), vesicles, cervical adenopathy. Exanthema. Desquamation | IVIG (3 doses), ASA, steroids. LMWH | ASA and acenocoumarol. Statins |
ASA, acetylsalicylic acid; GCA, giant coronary aneurysm; IVIG, intravenous immunoglobulin; LAD, left anterior descending coronary artery; LMWH, low-molecular-weight heparin; LVEF, left ventricular ejection fraction; RCA, right coronary artery; r-TPA, recombinant tissue plasminogen activator.
In the 2 cases with coronary thrombosis (cases 1 and 3), antiplatelet treatment with ASA was supplemented with anticoagulant therapy with subcutaneous low-molecular-weight heparin or IV heparin sodium. In addition, since these patients continued to have elevated inflammatory markers and a considerable baseline hypercoagulability that did not improve adequately with anticoagulant therapy, they were also given steroids and additional anti-inflammatory agents, such as infliximab; treatment with r-TPA was prescribed in both patients and maintained for 12h to little effect, followed by IV heparin sodium, which was effective.
Asymptomatic intra-aneurysmal thrombosis was detected in one patient (case 3), initially by echocardiography and later by CCTA (Fig. 2) with origin in the right coronary artery (RCA), with a maximum diameter of 13mm, and in the ostial left anterior descending coronary artery (LAD). The patient received systemic thrombolytic therapy with r-TPA, infliximab, abciximab and IV heparin, and had mild systolic dysfunction. Magnetic resonance with IVPD confirmed that the thrombus was old due to the presence of necrosis in the septal and posterior regions and of collateral vessels in some areas. Treatment with ASA, acenocoumarol, angiotensin-converting enzyme inhibitors, carvedilol and spironolactone continued after discharge.
Another patient (case 1) received a diagnosis of intra-aneurysmal thrombosis in the RCA, with prescription of IV heparin sodium and r-TPA, and evidence of mild systolic dysfunction in the left ventricular ejection fraction (LVEF). Follow-up echocardiograms showed that the thrombus had dissolved and the LVEF had normalised, the follow-up CCTA confirmed the absence of intra-aneurysmal thrombotic lesions, and MRI with IVDP ruled out the presence of ischaemic or necrotic lesions and evinced the normalisation of LVEF. The treatment prescribed at discharge was prophylactic antithrombotic therapy and captopril as the sole therapy for myocardial function.
On average, coronary lesions were detected more than 10 days from the onset of fever, although it must be taken into account that most patients were referred from other facilities. Even so, none of the patients developed severe LVEF impairment, severe valvulopathies or mechanical complications during the acute phase. During the follow-up, coronary lesions remained stable without development of new complications (stenosis oraneurysms).
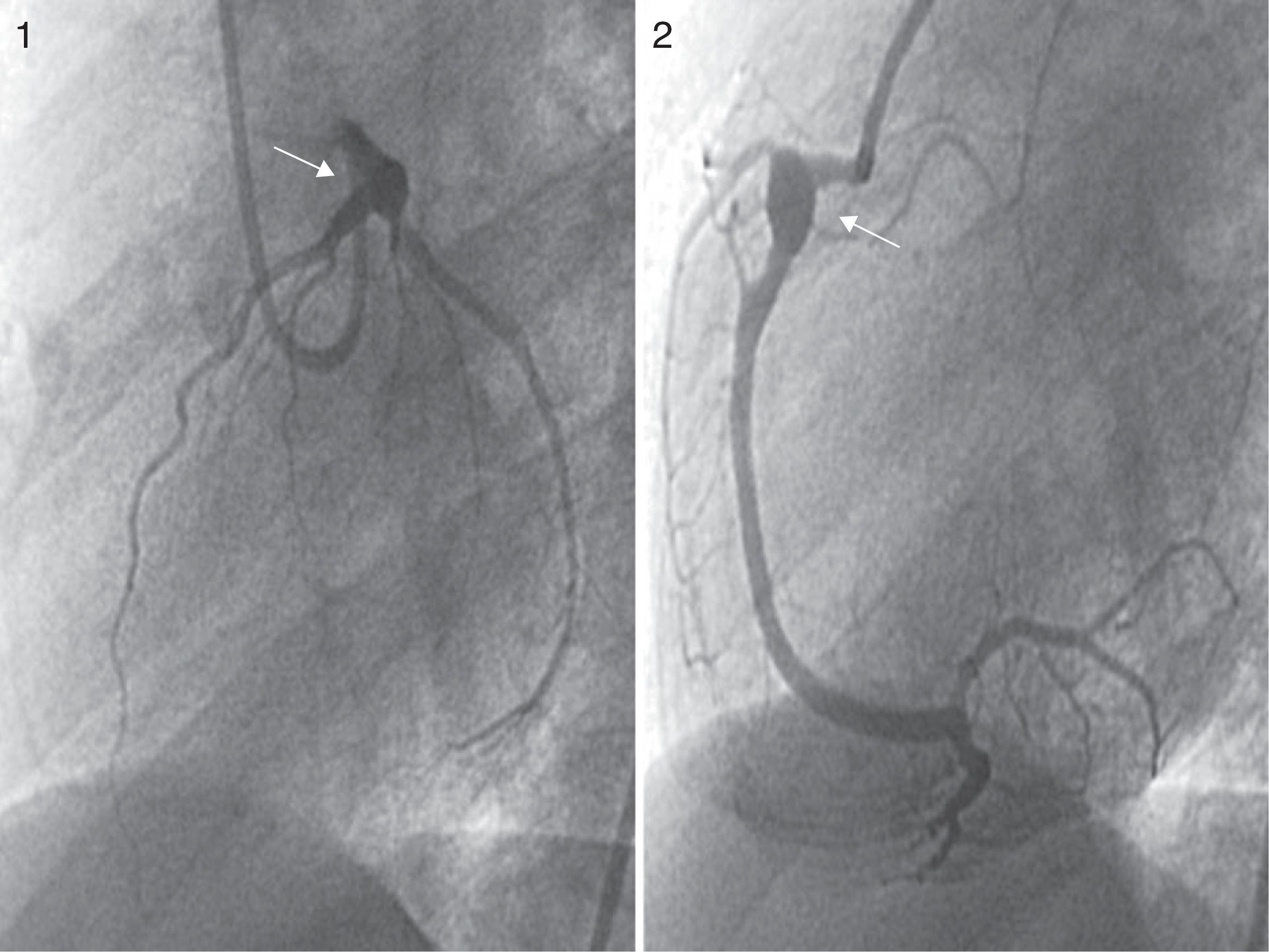
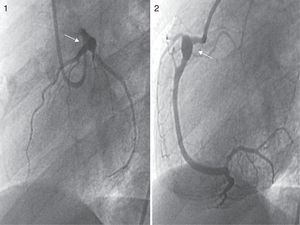
Patients made periodic follow-up visits on an outpatient basis that included electrocardiography, echocardiography every 3–6 months and CCTA every 12 months, and at least one myocardial perfusion scan (earlier cases) or a MRI scan with IVDP (Fig. 3) to assess function for the purposes of prognostication, which was repeated periodically in the 2 patients that had coronary thrombosis. A coronary angiogram was performed in the 3 earliest patients and in the 2 recent patients with intracoronary thrombosis after the initial phase of the disease (Fig. 4). The first 3 patients underwent ergometric stress testing, which they tolerated well, with normal findings in all.
Aneurysmal lesions persist in all patients to date, and they remain under chronic treatment with ASA at antiplatelet doses, acenocoumarol to maintain the INR in the 2–2.5 range. Three patients (cases 3, 4 and 8) have also received hypolipidemic therapy with statins at some point of the follow-up (mean age at treatment initiation, 8.25 years).
DiscussionEarly suspicion of KD continues to be essential to improve the long-term prognosis of these patients, as early treatment with IVIG and ASA at anti-inflammatory doses is the most important factor in preventing the development of CAs, which generally form between days 7 and 10 of fever and are the main cause of cardiovascular-related morbidity and mortality in KD. Early treatment reduces morbidity and mortality to 2–12% from 25%, and the incidence of giant aneurysms to less than 1% from 4%.4,7,8 The median time of treatment initiation in our series was day 12 of fever, which is a relevant negative predictor for the development of coronary abnormalities and for the response to the initial immunoglobulin dose. The administration of a second dose of IVIG combined with initiation of steroid treatment is indicated in patients that do not exhibit a full response to IVIG within 36h.9,10 A recent study reported good outcomes in patients with KD at high risk of coronary lesions treated with a combination of IVIG and prednisone that was maintained until CRP levels normalised.11–13 However, the efficacy and optimal regimen for steroid therapy have yet to be determined (methylprednisolone pulses are the preferred treatment at present), and the same is true of the indications GP IIB/IIIA inhibitors like abciximab and new-generation anti-inflammatory drugs like infliximab,14 which are currently being used in severely ill patients with giant CAs and/or ventricular dysfunction with thrombotic complications that do not respond to repeated IVIG doses.15,16 In our study, patients required at least 2 doses of immunoglobulin to become afebrile, in 5 cases with the addition of steroids, and with the most severe cases requiring new therapies such as abciximab or infliximab. The 2 cases of KD with intracoronary thrombosis corresponded to high-risk patients with a late diagnosis in whom persistence of fever and of the baseline state of hypercoagulability promoted the development of these complications. It is essential that efforts are being made not only to prevent but also to control inflammation, as it provides a basic substrate for the development of thrombi in a high-risk area.
Echocardiography is the essential tool for the diagnosis and follow-up of cardiac lesions, accompanied by electrocardiography. Today, the size of CAs is routinely assessed using z-score tables for coronary artery diameters normalised for body surface area. All our patients underwent echocardiographic examination for diagnosis and follow-up, and this technique was also used in the early assessment of complications. Coronary CT angiography is a valuable tool in the diagnosis and follow-up of these patients, but the associated exposure to ionising radiation and the need for anaesthesia and heart rate regulation must be taken into account; given its availability, speed and the amount of information it provides, it has become the ideal technique to replace coronary angiography, which carries a higher risk due to coronary involvement in these patients.9 Coronary angiography was only performed in the earliest patients in the series, while more recent patients were assessed by means of CCTA for the purpose of and during the follow-up. We performed a follow-up CCTA at 1 year from diagnosis unless the results of noninvasive tests called for performing it at an earlier time. When it comes to function tests, MRI with IVDP provides valuable information on myocardial viability and for the assessment of aneurysms; it requires sedation or anaesthesia in young patients, while its key advantage is the absence of radiation exposure.12 Coronary angiography affords a precise definition of aneurysms, stenosis, thrombosis with blood flow obstruction and collateral blood flow. At present, its use is restricted to the few cases in which other imaging techniques have not been helpful, patients with chronic symptomatic lesions, for revascularization procedures or patients with subclinical obstruction that test positive for ischaemia.16,17 MRI with IVDP was only performed in the most recent patients in the series to complete the evaluation after CCTA; during the follow-up, this test was performed at 6 months and then 1 year after in patients that had lesions at the time of diagnosis, and subsequently based on the condition of the patient. Current recommendations for the follow-up of patients with CAs include performance of an echocardiogram and ECG every 2–4 months and an evaluation of ischaemia by means of a stress test or MRI with IV dipyridamole every 6–12 months or whenever patients exhibit symptoms indicative of ischaemia.18,19
The duration of fever, which may reflect the development of inflammatory vascular damage, has been associated with an increased risk of clinically significant coronary lesions. There is evidence of an increased incidence of coronary complications when fever persists for more than 7 days. Harada et al.20 established a set of criteria to determine the risk of coronary lesions in patients with KD in order to identify those most at risk of coronary involvement that would benefit from IVIG therapy. These criteria include white blood cell count of more than 12,000/mm3, platelet count of less than 350,000/mm3, serum CRP of less than 30mg/L, haematocrit of less than 35%, albumin of less than 3.5g/dL, age of less than 12 months and male sex.
Once the acute phase is over, the goal of treatment is to decrease the risk of coronary thrombosis. Late changes in coronary lesions have an impact on recovery and the development of fibrosis in the affected arteries and may result in stenosis, especially in the segment previously affected by the aneurysm, increasing the risk of thrombosis, acute myocardial infarction and sudden death. There are descriptions in the literature of patients that develop progressive intimal hyperplasia years after the initial episode of KD. Patients with mild persistent coronary lesions (ectasias or small aneurysms) will remain on antiplatelet therapy at minimum. It is recommended that the follow-up of patients with giant CA aneurysms include antiplatelet therapy with ASA and anticoagulation therapy with acenocoumarol to maintain the INR in the 2–2.5 range for an indefinite period of time.21 The fact that coronary lesions in KD differ from those found in atherosclerosis in adults should be taken into account.22 Traditionally, complications have been treated by surgical myocardial revascularization due to the considerable risks associated to percutaneous coronary intervention in these patients. To date, none of our patients has required revascularization treatment.
Patients with KD experience subclinical changes in endothelial function and fractional flow reserve,23 so they seem to be at higher risk of cardiovascular problems compared to healthy children, and have higher blood pressures and increased adiposity that persist through adulthood. Thus, it is essential that these patients remain in follow-up with implementation of measures for the secondary prevention of ischaemic heart disease.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Sánchez Andrés A, Salvador Mercader I, Seller Moya J, Carrasco Moreno JI. Aneurismas coronarios gigantes en lactantes con enfermedad de Kawasaki. An Pediatr (Barc). 2017;87:65–72.