Antibiotics represent one of the most widely prescribed therapeutic agents in children. It has been estimated that 30–50% of antibiotic prescriptions for this population are inappropriate. In this scenario, analysis of prescription data provides an invaluable source of information as a basis for implementing strategies for improvement in this field.
ObjectiveTo assess the appropriateness of antibiotic prescriptions in a paediatric population at an emergency department.
MethodsAn observational, descriptive, and cross-sectional study was conducted on patients under 14 years who attended the emergency department during 2013. A random sample of 630 patients was selected (confidence level 99%, accuracy 5%). To assess the suitability of antibiotic prescriptions, the clinical practice was compared with an evidence-based guideline especially designed for this study.
ResultsAntibiotics were prescribed to 16.5% patients (n=104). Antibiotic treatment was inappropriate in 51.9% patients (n=54). Unnecessary treatment was indicated in 40.7%, with wrong antibiotics chosen in 35.2%, and the posology was incorrect in 24.1% of them. The most frequent diseases with incorrectly prescribed antibiotics were: acute otitis media, episodes of wheezing, fever of unknown origin, acute pharyngo-tonsillitis, and community-acquired pneumonia.
ConclusionAntibiotic prescribing seems to be inappropriate in up to half of the patients. These data reinforce the need to develop a paediatric antimicrobial stewardship programme to decrease the unnecessary use of antimicrobial agents.
Los antimicrobianos son uno de los agentes terapéuticos más empleados en niños. Se estima que entre el 30 y el 50% de las prescripciones son inadecuadas. En este escenario, el análisis de la prescripción aporta información importante para la implementación de medidas de mejora en este campo.
ObjetivosEvaluar la adecuación de la prescripción de antimicrobianos en población pediátrica en un servicio de urgencias.
MétodosEstudio observacional, descriptivo y transversal en población menor de 14 años atendida en las urgencias hospitalarias de un hospital comarcal durante el año 2013. Se seleccionó una muestra aleatoria de 630 pacientes (intervalo de confianza: 99%; error alfa: 5%). Se analizó el grado de adecuación del tratamiento antimicrobiano comparando nuestra práctica clínica con las recomendaciones de una guía de tratamiento antimicrobiano basada en la mejor evidencia disponible diseñada especialmente para este estudio.
ResultadosSe prescribió antimicrobiano al 16,5% de los pacientes (n=104). El tratamiento fue considerado inadecuuado en el 51,9% de los pacientes (n=54). Se prescribió tratamiento innecesario en el 40,7%, la elección del antimicrobiano fue incorrecta en el 35,2% y la posología en el 24,1%. Las principales enfermedades en las que se produjo la prescripción inadecuada fueron: otitis media aguda, episodio de sibilancias, fiebre sin foco, faringoamigdalitis aguda y neumonía adquirida en la comunidad.
ConclusiónHasta en la mitad de los pacientes la prescripción de antimicrobianos puede ser inadecuada. Estos resultados ponen de manifiesto la importancia de introducir un programa de optimización de antimicrobianos para reducir su uso innecesario.
Infectious diseases are one of the most frequent reasons for seeking emergency care in the paediatric population. It is estimated that 2 out of 3 children that visit the emergency department do so in relation to infectious diseases.1,2 Antibiotic agents are among the most frequently prescribed drugs, and Spain is one of the countries in Europe with the highest rate of antibiotic consumption in the community (outside hospitals).3 Previous studies in the paediatric population have found that antibiotic agents are prescribed in 12%–18% of paediatric emergency visits.4,5
There is a high percentage of inappropriate antibiotic prescription both in hospitals and in the community. It is estimated that prescription of these drugs may be inappropriate in up to 30%–50% of cases.6,7 Acute paediatric disease is particularly conducive to inappropriate prescription of antibiotic agents. A high proportion of patients seek care for respiratory infections, and these diseases are the main reason for inappropriate use.8,9 Other factors include high caseloads, diagnostic and aetiologic uncertainty, difficulties in following up patients after discharge, and the low availability, in general, of rapid microbiological tests to determine whether the disease has a bacterial or a viral aetiology.10 The high and inappropriate consumption of antibiotic agents results in increased antimicrobial resistance at both the population and the individual levels.11 Furthermore, it can give rise to drug-related adverse events, changes in the body's microbiota, sensitisation with potential for future allergy and an increased risk of asthma or obesity.12,13
The problems that result from the inappropriate use of antibiotics have been recognised by scientific, health care and policy-making institutions. This has led to the development of strategies such as antimicrobial stewardship programmes (ASPs), which aim at improving antibiotic prescription with the end of achieving better clinical outcomes, reducing the incidence of adverse events associated with inappropriate use, and increasing the cost-effectiveness of care.14,15
Given that a large proportion of antimicrobial treatments are inappropriate and therefore unnecessary, we believe that a thorough knowledge of the actual pattern of use in each care setting would be of great interest to understand the circumstances under which inappropriate prescription occurs as well as its causes, with the ultimate purpose of implementing quality improvement interventions to achieve appropriate antimicrobial prescription.16–18
The aim of this study was to assess whether antibiotics were used inappropriately in the paediatric population at the emergency department of our hospital and to identify the diseases associated with inappropriate use as well as the factor in which the use was inappropriate: indication for use, choice of drug, dose, interval between doses or duration of treatment. To our knowledge, this is the first study of these characteristics conducted in the emergency department of a regional hospital.
Materials and methodsWe conducted a cross-sectional, observational descriptive study to measure the appropriateness of antibiotic prescription in children aged less than 14 years managed at the emergency department of the Hospital de la Merced in Osuna (Seville, Spain) in 2013. In this department, emergency visits are managed by family physicians and interns in family medicine, in consultation with paediatricians. The department serves patients with medical, orthopaedic or surgical conditions. Of the 12,503 paediatric emergency visits received in the year under study, we randomly selected a sample of 630 patients (sample size calculated for an alpha error of 5% with a 99% confidence interval and an expected proportion of 50%). Dates of service were chosen at random, and we included all patients that visited the department on those dates and were discharged home until we reached the established sample size. We excluded patients that were admitted to hospital and patients referred to other hospitals.
The primary outcome in our study was whether antibiotic prescribing was appropriate or inappropriate. We defined inappropriate use as prescription of an antibiotic for a disease for which antibiotherapy is not indicated, selection of an antibiotic that is neither the drug of choice or the alternative drug indicated for the disease, or prescription of an inappropriate dose, interval between doses or duration or treatment.
To assess the appropriateness of the indication, choice of antibiotic and dosage, we compared the prescribed treatment with a guideline for empirical antimicrobial treatment developed in the Osuna Health Area to be introduced in our hospital in the future. This guideline was based on the ABE guideline on infectious diseases,19 several consensus documents of the Asociación Española de Pediatría (Spanish Association of Pediatrics)20–25 and the second edition of the guideline for antimicrobial treatment of the Aljarafe health district.26
The variables under study were: age, sex, comorbidities, allergy to antimicrobials, antibiotic use before emergency visit, diagnosis at discharge, antibiotic prescription, type of antibiotic prescribed, dose, interval between doses, and duration of treatment.
We performed a descriptive analysis of the variables under study. We summarised qualitative variables as absolute frequencies and percentages, and quantitative variables as mean and standard deviation or, in case of an asymmetrical distribution, median and interquartile range (IQR). We compared qualitative variables by means of the chi square test. A p-value of less than 0.05 in any of the tests was considered statistically significant. We performed the statistical analysis with Microsoft Excel 2007.
ResultsThe median age of the patients was 3.3 years (IQR, 1.4–8.8 years). The male-to-female ratio was 1.2:1. There were comorbidities in 14.9% of the patients (n=94), the most frequent of which were asthma and recurrent wheezing. Of all patients, 2.5% (n=16) reported allergies to antibiotics, most commonly to penicillin (1.7%). Patients were already receiving antibiotic treatment at the time of the visit in 7.8% of cases (n=49). The most frequent antibiotics in these patients were amoxicillin and amoxicillin–clavulanic acid, which were both taken by 36.7%.
Of the 630 selected patients, 45.9% (n=289) had a discharge diagnosis whose aetiology was most probably infectious. Antibiotic treatment was prescribed in 16.5% (n=104) of the patients included in the study. The antibiotics used, in decreasing frequently, were amoxicillin–clavulanic acid (29.8%), amoxicillin (27.9%), azithromycin (16.4%), cefixime (5.8%), clarithromycin (1.9%) and others (18.2%). We considered that antimicrobial treatment was inappropriate in 51.9% of cases (n=54).
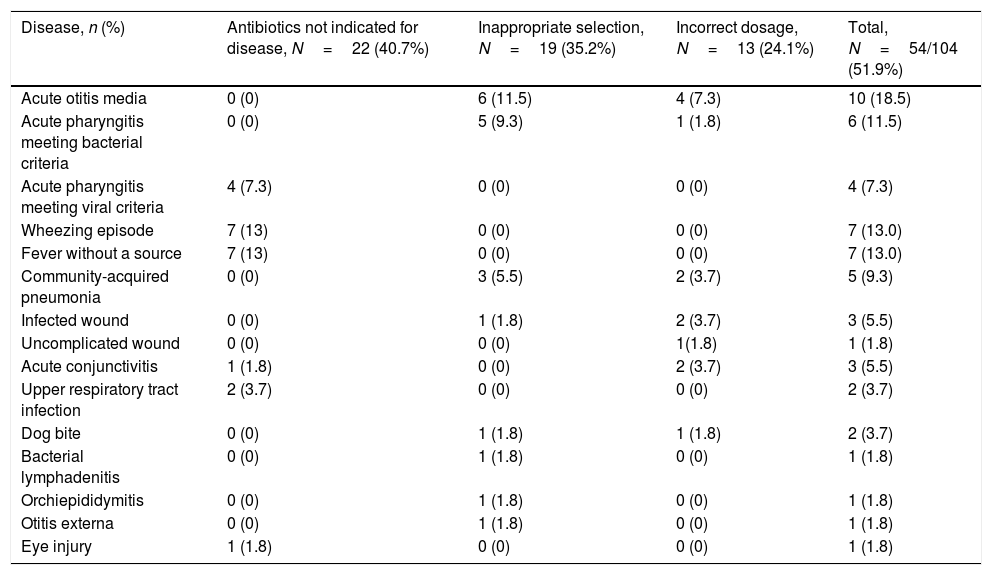
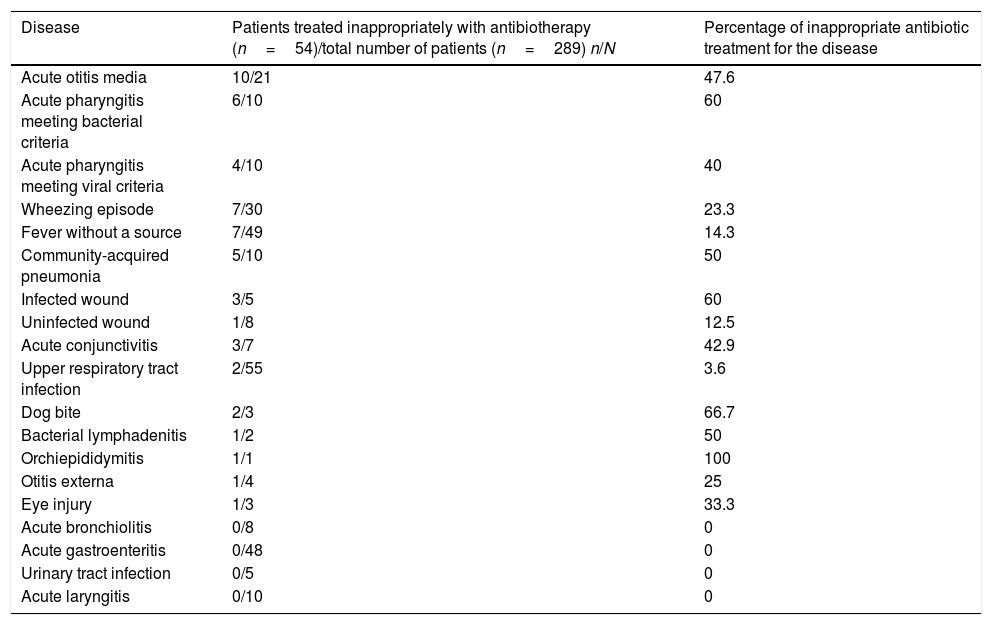
Table 1 summarises the diseases and the dimension in which antibiotic use was inappropriate. The reasons why treatment was inappropriate were: disease for which antibiotherapy was not indicated (40.7%; n=22), inappropriate selection of antibiotic agent (35.2%; n=19) and dosage errors (24.1%; n=13). Of the dosage errors, 4 corresponded to inappropriate doses, 2 to inappropriate intervals between doses, and 7 to inappropriate duration of treatment. In one case there were 2 dosage errors. Table 2 presents the percentage of inappropriate antibiotic use by disease.
Diseases treated inappropriately with antibiotherapy and reason why the treatment was inappropriate.
| Disease, n (%) | Antibiotics not indicated for disease, N=22 (40.7%) | Inappropriate selection, N=19 (35.2%) | Incorrect dosage, N=13 (24.1%) | Total, N=54/104 (51.9%) |
|---|---|---|---|---|
| Acute otitis media | 0 (0) | 6 (11.5) | 4 (7.3) | 10 (18.5) |
| Acute pharyngitis meeting bacterial criteria | 0 (0) | 5 (9.3) | 1 (1.8) | 6 (11.5) |
| Acute pharyngitis meeting viral criteria | 4 (7.3) | 0 (0) | 0 (0) | 4 (7.3) |
| Wheezing episode | 7 (13) | 0 (0) | 0 (0) | 7 (13.0) |
| Fever without a source | 7 (13) | 0 (0) | 0 (0) | 7 (13.0) |
| Community-acquired pneumonia | 0 (0) | 3 (5.5) | 2 (3.7) | 5 (9.3) |
| Infected wound | 0 (0) | 1 (1.8) | 2 (3.7) | 3 (5.5) |
| Uncomplicated wound | 0 (0) | 0 (0) | 1(1.8) | 1 (1.8) |
| Acute conjunctivitis | 1 (1.8) | 0 (0) | 2 (3.7) | 3 (5.5) |
| Upper respiratory tract infection | 2 (3.7) | 0 (0) | 0 (0) | 2 (3.7) |
| Dog bite | 0 (0) | 1 (1.8) | 1 (1.8) | 2 (3.7) |
| Bacterial lymphadenitis | 0 (0) | 1 (1.8) | 0 (0) | 1 (1.8) |
| Orchiepididymitis | 0 (0) | 1 (1.8) | 0 (0) | 1 (1.8) |
| Otitis externa | 0 (0) | 1 (1.8) | 0 (0) | 1 (1.8) |
| Eye injury | 1 (1.8) | 0 (0) | 0 (0) | 1 (1.8) |
Inappropriate antibiotic treatment by disease.
| Disease | Patients treated inappropriately with antibiotherapy (n=54)/total number of patients (n=289) n/N | Percentage of inappropriate antibiotic treatment for the disease |
|---|---|---|
| Acute otitis media | 10/21 | 47.6 |
| Acute pharyngitis meeting bacterial criteria | 6/10 | 60 |
| Acute pharyngitis meeting viral criteria | 4/10 | 40 |
| Wheezing episode | 7/30 | 23.3 |
| Fever without a source | 7/49 | 14.3 |
| Community-acquired pneumonia | 5/10 | 50 |
| Infected wound | 3/5 | 60 |
| Uninfected wound | 1/8 | 12.5 |
| Acute conjunctivitis | 3/7 | 42.9 |
| Upper respiratory tract infection | 2/55 | 3.6 |
| Dog bite | 2/3 | 66.7 |
| Bacterial lymphadenitis | 1/2 | 50 |
| Orchiepididymitis | 1/1 | 100 |
| Otitis externa | 1/4 | 25 |
| Eye injury | 1/3 | 33.3 |
| Acute bronchiolitis | 0/8 | 0 |
| Acute gastroenteritis | 0/48 | 0 |
| Urinary tract infection | 0/5 | 0 |
| Acute laryngitis | 0/10 | 0 |
When we analysed factors such as the time of day and season of the year that the patients received care or whether patients were already using antibiotics at the time of the visit, we found no statistically significant differences in the proportion of antibiotic prescription nor its appropriateness.
DiscussionWe present a study on the quality of antibiotic prescribing in the paediatric population conducted in the emergency department of a regional hospital. To assess the appropriateness of the indication, selection of antibiotic and dosage, we used a guideline for empirical antibiotic treatment developed in the Osuna health area of Andalusia that was going to be introduced in our hospital as the reference guideline in the future. The decision to establish our own guideline for antimicrobial treatment was based on current recommendations for the development of ASPs. These recommendations suggest that it is preferable that each hospital develop its own protocols for prophylactic, empirical and targeted antibiotic treatment in order to not only take into account the recommendations given by scientific societies, but also the peculiarities of each hospital, the local epidemiology and all the medicine specialties that may be involved, all of which promotes acceptance of the guideline and future adherence to it.14
In our study, we found a percentage of inappropriate antibiotic prescribing of 51.9%. This figure is very similar to those reported in studies on the quality of antibiotic prescribing in the adult population.14 When it comes to studies in the paediatric population in Spain, it is difficult to compare reported percentages due to the heterogeneity in their methodology. A study on the quality of antibiotic prescribing in patients with acute otitis media, acute pharyngitis or community-acquired pneumonia conducted in the paediatric emergency department of a tertiary level hospital found inappropriate antibiotic treatment in 22.3%.1 The ABES study, which analysed the appropriateness of the empirical selection of antibiotics by Spanish paediatricians, found that the selection was inappropriate in 15.2% of cases based on current protocols, clinical guidelines and consensus documents. The rate of inappropriate prescription was 10% for diseases that required hospital admission and 23% for diseases that did not require admission and were managed only at the outpatient level. This study considered only the selection of the antibiotic agent and not the dosage, and it was not based on data from actual prescriptions but on self-reports of hypothetical use.27 A multicentre study on the appropriateness of antibiotic prescribing in patients with respiratory disease managed in several paediatric emergency departments reported a proportion of inappropriateness of 36%.9
We found that the most frequent reason why prescribing was inappropriate was the use of antibiotherapy in infectious diseases for which this treatment is not indicated. The second most frequent reason was selection of an inappropriate antibiotic agent. In most cases, this corresponded to the selection of amoxicillin–clavulanic as opposed to amoxicillin in infections where clavulanic acid did not provide any added benefit, such as acute pharyngitis or typical pneumonia.23 There were also cases of inappropriate selection where azithromycin was used as the first-line agent for treatment of infections for which it is not the drug of choice, such as acute pharyngitis, acute otitis media or typical community-acquired pneumonia. The negative repercussions of their inappropriate use include not only the development of antimicrobial resistance, but also a risk of treatment failure due to the high prevalence of resistance in bacteria such as pneumococcus species or Streptococcus pyogenes, or its suboptimal efficacy against Haemophius influenza.28 When it came to dosage errors, and consistently with other studies, the most frequent type was inappropriate duration of treatment. There is a tendency to prescribe regimens that are shorter than recommended, especially in cases of acute pharyngitis. The main reason for this is the tendency to prescribe 7-day courses of treatment by default for any type of infection, failing to take into account that this is not appropriate for every infectious disease or every antibiotic agent.1,5,6
The prevalence of antibiotic prescribing in our study was consistent with the prevalence reported in other studies conducted in Spain.1,5,29 The existing literature evinces considerable differences in antibiotic use between countries and between geographical areas within countries. One systematic review found that the prevalence of antibiotic use was up to 4 times higher in the countries with the highest consumption compared to the countries with the lowest consumption.30
As for the distribution of antimicrobial agents, we found that the most frequently used type was broad-spectrum penicillins combined with a beta-lactamase inhibitor (amoxicillin–clavulanic acid), followed by broad-spectrum penicillins (amoxicillin). When combined, these two drugs account for more than half of antibiotic prescriptions. It is worth highlighting that, as found in previous studies, amoxicillin–clavulanic was the most frequently used antimicrobial rather than amoxicillin, which is the drug of choice for most respiratory infections.1,9 The current evidence shows that countries with the highest rates of antibiotic use are also the countries with the highest use of amoxicillin–clavulanic acid. Conversely, countries with a lower use of antibiotics correspond to the countries where amoxicillin is the most frequently prescribed antimicrobial. This reveals that appropriate prescribing is usually associated with a lower consumption of antimicrobials.30 We found a much greater use of macrolides in our study compared to the use described by other studies conducted in Spain, which ranged from 5% to 10%. This finding may be indicative of a low adherence to antimicrobial treatment protocols and guidelines, as macrolides are only recommended for use as first-line treatment in exceptional cases and are usually reserved for patients allergic to beta-lactam antibiotics. The use of cephalosporin, on the other hand, was consistent with the use reported by other authors.1,5,29
The diseases where the inappropriate use of antibiotics was most frequent were acute otitis media and acute pharyngitis. In the case of otitis media, we added the recommendations of the consensus document on the aetiology, diagnosis and treatment of otitis media developed by Del Castillo et al.24 to our own guideline for the purpose of assessing the appropriateness of antibiotic prescribing. The percentage of inappropriate use of antibiotics was of 47.6%, above the percentages reported in previous studies in Spain, which are usually of approximately 30%. Inappropriate use most frequently corresponded to prescription of amoxicillin–clavulanic acid in patients meeting the criteria for initial treatment with amoxicillin.24 As for pharyngitis, we ought to highlight that none of the patients that had it were treated with oral penicillin, despite it being the antibiotic of choice still recommended by current guidelines, as there is no evidence to date of S. pyogenes strains developing resistance to penicillins.31 This phenomenon has been found in most of the studies conducted in Spain and in other Mediterranean countries, in opposition to the findings of studies in Northern Europe.1,9,30 We found that antibiotherapy was used in 40% of patients with pharyngitis of a probable viral aetiology. The use of scales such as the McIsaac score and tests for the rapid detection of S. pyogenes can help optimise antimicrobial treatment in cases of pharyngitis.32,33
Fever without a source was treated incorrectly in 14.3% of patients presenting with this condition. Most episodes of fever without a source are caused by viral agents, so the decision whether to treat them with empirical antibiotherapy must be based on the patient's age, immune status and disease severity suggested by the clinical presentation (disease severity scales), or when the results of diagnostic tests, when applicable, suggest a bacterial aetiology.34,35
We found variability in the degree of inappropriate antibiotic prescribing in other respiratory infections of probable viral aetiology. Episodes of wheezing likely to be caused by a virus were treated inappropriately with antibiotics in 23.3% of cases. The reported percentages of antimicrobial prescription in these diseases range from 11% to 45%.9,29 The percentage of inappropriate antibiotic prescribing for upper respiratory tract infections was 3.6% in our study, lower than reported by other authors. Some studies have found that antibiotics were used to treat this disease in as many as 40%–50% of cases.36 Not using antibiotics to treat upper respiratory tract infections is considered an indicator of quality care. Community-acquired pneumonia is usually managed appropriately in emergency departments. Previous studies in Spain have found high percentages of appropriate ranging from 85% to 91%.1,9 The percentage of appropriateness we found in our study was lower, of 50%.1,9 The main contributors to this were the use of amoxicillin–clavulanic acid and of amoxicillin at a dose of 50mg/kg/day. Most consensus documents recommend a dose of 80mg/kg/day, and it is possible that the decreasing trend in the prevalence of penicillin resistance in circulating pneumococcal species and the good penetration of oral beta-lactam antibiotics into the inflamed lung will eventually make a dose of 50mg/kg/day appropriate, although it is not at present.37
The limitations of our work include the biases intrinsic to any retrospective study. It is possible that information bias affected our data, as some relevant information may have not been entered in the health records or discharge summaries. Another limitation is that the reference for comparison was a guideline for antimicrobial treatment that had not been introduced in our hospital at the time of the study.
To conclude, we would like to underscore the fact that antibiotic prescription was inappropriate in up to 50% of patients. Our data emphasise the importance of establishing an ASP in our hospital, the key elements of which would be the implementation of the antimicrobial use guideline developed for this study, educational interventions in the form of training courses and guidance on prescribed treatments, and periodic studies to survey the appropriateness of antibiotic prescription.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Croche Santander B, Campos Alonso E, Sánchez Carrión A, Marcos Fuentes L, Diaz Flores I, Vargas JC, et al. Adecuación de la prescripción de antimicrobianos en población pediátrica en un servicio de urgencias hospitalario. An Pediatr (Barc). 2018;88:259–265.