Perinatal palliative care (PC) services offer continuous and coordinated care for infants with life-limiting or life-threatening diseases from the time of diagnosis, frequently antenatal, through death and bereavement.1
In the Hospital Sant Joan de Déu of Barcelona, Spain, a perinatal PC programme was established in 2013 within the departments of gynaecology/obstetrics and neonatology, later integrated in 2017 in the new paediatric palliative care unit. The aim of our study was to assess the survival and place of death of the patients managed by the paediatric PC team within the perinatal PC programme and how families perceived the provided care.
We collected retrospective data from the electronic health records for the study variables. To assess the parental experience, we included the families of the neonates managed by the paediatric PC team who were born and died in our hospital. We used the Parental PELICAN Questionnaire (PaPeQu),2,3 in which the items, rated on a Likert scale, are distributed into 6 domains: communication, shared decision-making, relief of pain and other symptoms, continuity of care, end-of-life care and family and bereavement support. The study was approved by the ethics committee of the hospital.
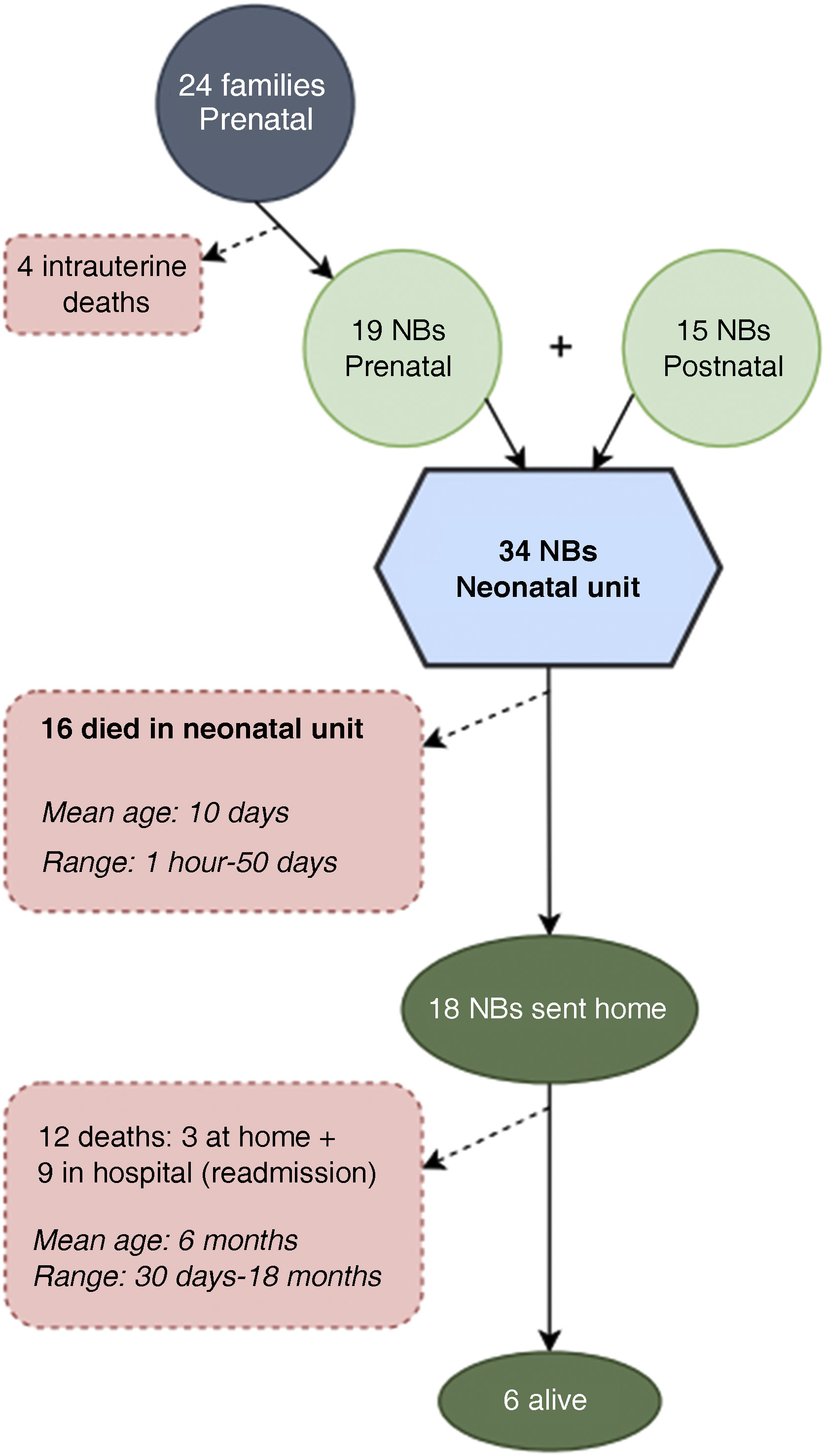
From January 2017 to December 2020, the paediatric PC unit provided care to 38 families within the perinatal PC programme: 23 (60.5%) were admitted to the programme before birth and 15 (39.5%) were referred at some point from the neonatal unit. The most frequent diagnoses were polymalformative syndromes (10 cases; 42%), followed by isolated disease of the central nervous system (8 cases; 21%), including holoprosencephaly, polymicrogyria and epileptic encephalopathy.
Fig. 1 presents the care history and outcomes of the patients. Of the 34 managed neonates, 16 (47%) died in the neonatal unit, 10 (29%) within 48 hours post birth (all had been admitted to the programme antenatally. The rest (18 newborns, 53%) were discharged home under follow-up by the paediatric PC team.
To assess the experience of families, we telephoned 15 families, out of which we obtained responses from 7 mothers: 5 had started follow-up by the paediatric PC team antenatally and 2 during the neonatal period.
Overall, families rated their experience very positively in all 6 domains (mean score out of a possible total of 6 points, 5.6; SD, 0.2), especially the domain of end-of-life care (mean, 5.8; SD, 0.2) and the continuity and coordination of care (mean, 5.7; SD, 0.4). The lowest score corresponded to communication with the care team (mean, 5.2; SD, 0.5), reflecting the parental perception that they had to actively seek clinical information or that they had not been prepared to handle the physical changes that could happen after death. On the other hand, all participants gave the highest possible score (6 points) to the item about being able to spend time and enjoy physical contact with their child at the end of life. Lastly, we asked parents to share their positive and negative experiences, which are summarised in Table 1.
Positive and negative experiences described by the parents.
| Positive experiences | Negative experiences | |
|---|---|---|
| Support to the family | Care, thoughtfulnessFeeling nurtured by health care providers | Long length of stay |
| Communication | The gynaecologist called the unborn baby by her name and did not just see her in terms of the diseaseCalm, supportive, respectful | I felt judged for my decision to continue with the pregnancyI was asked about my birth plan because they had not read itDoctors were indifferent to the news about additional malformations, justifying it by saying that it did “not change anything” |
| End-of-life care and bereavement support | The suggestion to take pictures To have her baptised and keep mementoes (album, health book, hand/footprints…) To reach out to other families | I was in the same ward where babies stayed when I no longer had my own baby |
The aim of describing these services in our study was to demonstrate the importance of specialised perinatal PC programmes offering continuous care from an early stage (during gestation in the case of an antenatal diagnosis) and adapted for a variable survival rate. More than half of the newborns in the programme could be brought home, a percentage that exceeded the percentage reported for similar programmes4,5 and that reflects the benefits of interdisciplinary coordination. The positive aspects of the programme were also reflected in the assessment made by the surveyed families, who expressed a high level of satisfaction with the care received.
On the other hand, we ought to highlight that the 16 newborns managed by the paediatric PC team who died in the neonatal unit amounted to 20% of the patients who died in the neonatal unit during the study period (total of 80). Most of the patients who died in the unit received palliative care from the neonatal care team without consultation with the paediatric PC team, which shows that the reasons for referral are multifactorial, including both the diagnosis and the timing of diagnosis, the prognosis and the clinical course of the disease and sociocultural characteristics as well as the acceptance of families.6
The main limitations of the study were the retrospective design of the descriptive analysis, the small sample size and the risk of selection bias in the survey.
In conclusion, the experience with the programme that we have described in addition to the highly positive perception by the families can support the development of perinatal PC services throughout Spain, promoting the institution of interdisciplinary programmes to improve care delivery.