Few validated surveys measuring parental satisfaction in the Paediatric Intensive Care Unit (PICU) are available, and none of them in Spanish language. The aim of this study is to translate and validate the questionnaire EMpowerment of PArents in THe Intensive Care (EMPATHIC). This questionnaire measures parental perceptions of paediatric intensive care-related satisfaction items in the Spanish language.
Material and methodsA prospective cohort study was carried out using questionnaires completed by relatives of children (range 0–17 years old) admitted into a tertiary PICU. Inclusion criteria were a length of stay more than 24h, and a suitable understanding of Spanish language by parents or guardians. Exclusion criteria were re-admissions and deceased patients. The questionnaire was translated from English to Spanish language using a standardised procedure, after which it was used in a cross-sectional observational study in order to confirm its validity and consistency. Reliability was estimated using Cronbach's α, and content validity using Spearman's correlation analysis.
ResultsA total of 150 questionnaires were collected. A Cronbach's α was obtained for domains greater than 0.7, showing a high internal consistency from the questionnaire. Validity was measured by correlating 5 domains with 4 general satisfaction items, documenting an adequate correlation (Rs: 0.41–0.66, p<.05).
ConclusionsThe Spanish version of EMPHATIC 30 is a feasible, easy, and suitable tool in this specific environment, based on the results. EMPATHIC 30 is able to measure parental satisfaction, and may serve as a valid indicator to measure quality of care in Spanish PICUs.
Existen pocas encuestas validadas para medir la satisfacción de los padres en las Unidades de Cuidados Intensivos Pediátricos (UCIP) y ninguna de ellas en idioma español. El objetivo de este estudio es traducir el cuestionario EMpowerment of PArents in THe Intensive Care (EMPATHIC), que mide la satisfacción y experiencias de los padres, a la lengua española y validarlo.
Material y métodosEstudio prospectivo, realizado en la UCIP de un hospital terciario mediante encuestas a los familiares de pacientes ingresados (de entre 0 y 17 años). Los criterios de inclusión fueron una estancia mayor de 24 h y una buena comprensión del idioma de los padres/tutores. Los criterios de exclusión fueron los reingresos y los pacientes fallecidos. Se realizó la traducción del cuestionario mediante un procedimiento estandarizado. Tras la traducción, se hizo un estudio observacional transversal para confirmar su validez y consistencia. La fiabilidad se estimó mediante el α de Cronbach y la validez de contenido mediante el análisis de correlación de Spearman.
ResultadosSe reunieron 150 encuestas. El α de Cronbach por dominios se situó por encima de 0,7, lo que indica una alta consistencia interna del cuestionario. La validez fue medida correlacionando los 5 dominios con los 4 ítems de satisfacción general, lo que demostró una correlación adecuada (rs: 0,41-0,66; p<0,05).
ConclusionesBasados en estos resultados, la adaptación del EMPHATIC-30 a la cultura e idioma español es un instrumento válido, de fácil cumplimentación y adecuado para el entorno estudiado, capaz de medir la satisfacción de los padres y de servir como guía para mejorar la calidad de la atención en las UCIP españolas.
Patient experience, assessed by means of satisfaction questionnaires, is currently considered a quality indicator in the field of “patient-centred care.”1,2 The importance of these questionnaires has been recognised for years as a means to ensure that the experiences and opinions of patients are heard and as useful tools for improving the quality of care.3–5
The concept of patient satisfaction extends to the families of patients,6 especially in young patients, where the approach of “patient-centred care” turns into “family-centred care.”7,8 Family satisfaction is assessed with the purpose of improving the quality and safety of care while promoting communication between families and health care staff. This is even more important in the paediatric intensive care units (PICUs), where the experience of a child's hospitalisation is particularly intense for families. Parental satisfaction with care is at the core of a framework grounded on respect for parental needs, adequate information, parental involvement in decision-making, physical and emotional support and coordination of care.5 Understanding the needs of parents is key to help make their experiences as bearable as possible.
All of the above evinces the need of having an effective tool to assess the perceptions of parents and their satisfaction with the care received by their children in the paediatric intensive care setting.5
Of all the questionnaires currently available to assess parental experience during the stay of children in paediatric intensive care units (PICUs), we chose the EMpowerment of PArents in THe Intensive Care (EMPATHIC-30) questionnaire developed by Latour (2013)9 to translate to Spanish and subsequently validate. This is a self-administered feedback form with 3 sections and 5 domains, such as care and treatment, parental participation and professional attitude. It was designed specifically to assess the experience and satisfaction of parents with the care received by their children in paediatric intensive care units (PICU).9
The aim of our study was to translate the original questionnaire (in English) to Spanish and validate the translation for its use as a benchmark of quality care in Spanish PICUs.
Materials and methodsThe EMPATHIC-30 is a shortened version of the initial EMPATHIC-6510 questionnaire developed in the Netherlands and validated through the study of 2 cohorts of parents/guardians of children hospitalised in several Dutch PICUs. It is a self-administered feedback form with 3 sections: the first for collection of general information on the patients and their parents, the second to assess parental experience during their child's stay in the PICU, and the third one to assess the overall experience throughout the patient's stay. It consists of 30 items organised into 5 domains: information (5 items), care and treatment (8 items), organisation (5 items), parental participation (6 items) and professional attitude (6 items). Responses are given on a 6-point Likert scale (1=highly disagree; 6=highly agree) with an additional “not applicable” answer option.
We translated the questionnaire following a structured method to ensure reliability. We applied the Principles of Good Practice for the Translation and Cultural Adaptation Process developed by the task force of the International Society for Pharmacoeconomics and Outcomes Research11 (ISPOR).
The process included the following steps:
- 1.
Initial preparation. We asked the author of the original questionnaire for permission and remained in touch with the author throughout the process to set the conceptual basis for the project.
- 2.
Translation of the original questionnaire to the target language by 2 independent translators employed in the field of health care and research.
- 3.
Reconciliation of the different translation versions by the research team.
- 4.
Back translation of the reconciled version into English by 2 translators that were native English speakers.
- 5.
Comparison and review of the different versions of the back translation against the original questionnaire, performed by the research team.
- 6.
Harmonization of all translations to ensure conceptual equivalence with the original, performed by the research team in consultation with the translators.
- 7.
Pilot test: we tested the translated questionnaire by giving it to 10 parents, who were also provided with an addendum for the purpose of recording any doubts that may arise with any of the items in regard to comprehension or wording and to assess how they perceived the questionnaire in general.
- 8.
Analysis of the results of the pilot test and completion of translation by the research team.
- 9.
Editing of questionnaire.
- 10.
Final report of the research team.
After translating the questionnaire following this process, we conducted an observational study. The study universe consisted of the parents or legal guardians of children discharged from the PICU of the Hospital Universitario de Cruces in Vizcaya. The PICU of the Hospital Universitario de Cruces is a medical-surgical 12-bed unit that admits approximately 600 patients per year. We selected patients by non-probability consecutive sampling until we obtained the desired sample size. The target was to obtain 150 individuals, with the calculation made for a 95% confidence interval and an error of 5%. The inclusion criteria were PICU stay longer than 24h and absence of language barriers. We excluded readmissions, parents/guardians that did not understand Spanish well, and parents of deceased children. We informed all the parents of the purpose of the study and requested their verbal consent for participation.
We gave the questionnaire to each family on the day their child was discharged from the unit and placed boxes for collection of completed questionnaires in the PICU and the inpatient wards.
Statistical analysisWe performed the statistical analysis of the data with the software SPSS 23.0 for Windows (SPSS Inc; 2003; Chicago, IL, USA). We assessed the reliability of the translated questionnaire by means of the Cronbach α (with a minimum acceptable value of 0.70) for each item and domain. We assessed internal consistency by calculating the Spearman correlation coefficient for the comparison of the 4 items that assessed general satisfaction (items used in every survey in the health care and manufacturing fields) and the 5 domains, considering the internal consistency acceptable if none of the items had a correlation coefficient of less than 0.4 and correlations statistically significant if the p-value was less than 0.05. In the descriptive analysis, we expressed quantitative variables as mean and standard deviation if they were normally distributed, and otherwise as median and interquartile range. We summarised qualitative variables as absolute frequencies and percentages. We defined statistical significance as a p-value of less than 0.05 for all the tests. The statistical analysis was performed by the research team in collaboration with the Unit of Clinical Epidemiology and Methodological Support of the hospital.
We obtained the approval of the Ethics and Research Committee of the Hospital Universitario de Cruces in Vizcaya. Since the data was anonymised, written informed consent was not required.
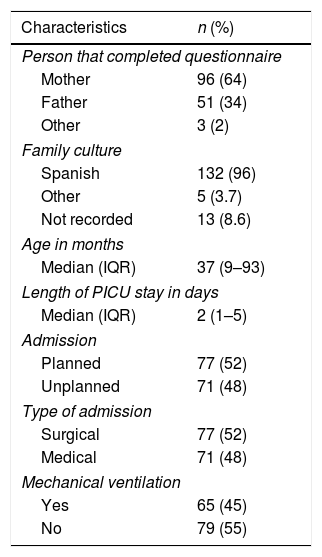
ResultsTable 1 summarises the characteristics of the patients and their parents. Sixty-four percent of questionnaires were completed by mothers, while 34% were completed by fathers. The median patient age was 37 months (interquartile range [IQR], 9–93). The median length of stay was 2 days (IQR, 1–5). We found no differences in the responses based on type of admission (planned/urgent), type of patient (surgical/medical) or the need for mechanical ventilation.
Characteristics of the children and their families.
| Characteristics | n (%) |
|---|---|
| Person that completed questionnaire | |
| Mother | 96 (64) |
| Father | 51 (34) |
| Other | 3 (2) |
| Family culture | |
| Spanish | 132 (96) |
| Other | 5 (3.7) |
| Not recorded | 13 (8.6) |
| Age in months | |
| Median (IQR) | 37 (9–93) |
| Length of PICU stay in days | |
| Median (IQR) | 2 (1–5) |
| Admission | |
| Planned | 77 (52) |
| Unplanned | 71 (48) |
| Type of admission | |
| Surgical | 77 (52) |
| Medical | 71 (48) |
| Mechanical ventilation | |
| Yes | 65 (45) |
| No | 79 (55) |
IQR, interquartile range.
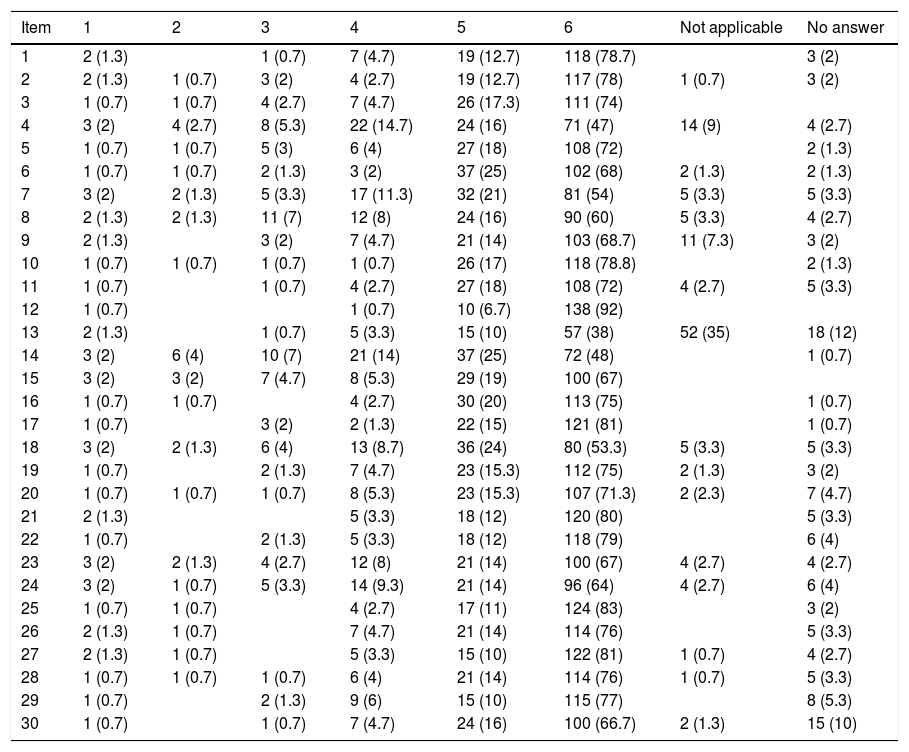
Appendix A shows the distribution of responses, expressed as absolute frequencies and percentages. Very few respondents picked the “not applicable” answer choice, except for item 13 (“It was easy to reach the PICU by phone”), which was marked as “not applicable” in 35% of completed questionnaires.
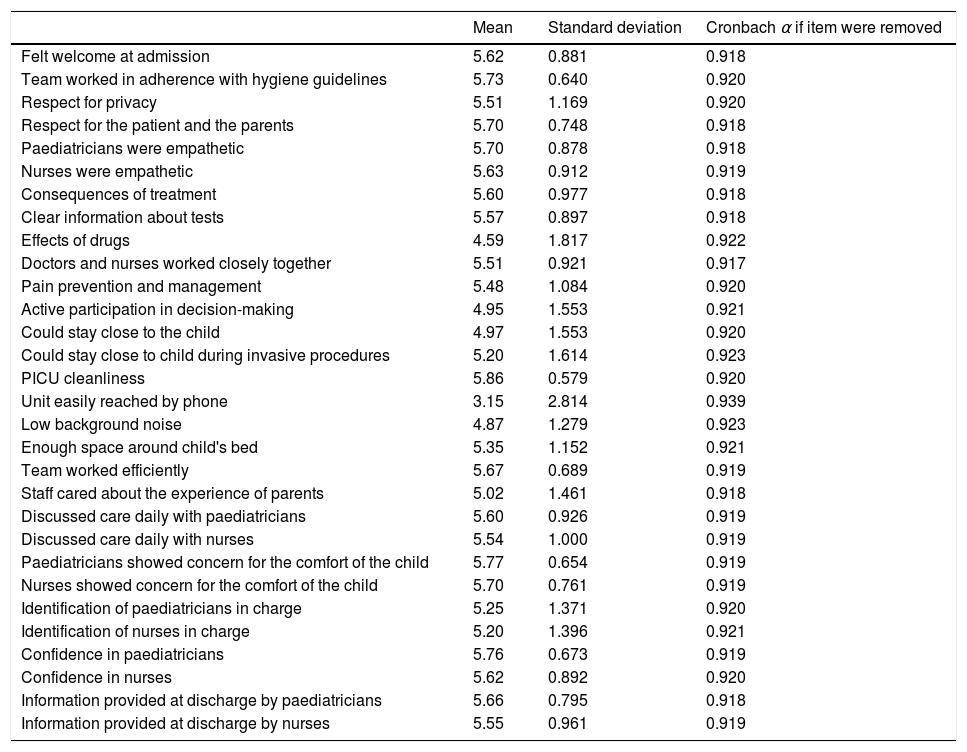
The mean score obtained in the 30 items exceeded 5, except for item “control of background noise in the unit,” which was 4.7 (SD, 1.47). We considered scores of more than 5 acceptable.
Table 2 presents the results of the descriptive analysis by item, mean and Cronbach α.
Descriptive analysis by item. Mean and Cronbach α.
| Mean | Standard deviation | Cronbach α if item were removed | |
|---|---|---|---|
| Felt welcome at admission | 5.62 | 0.881 | 0.918 |
| Team worked in adherence with hygiene guidelines | 5.73 | 0.640 | 0.920 |
| Respect for privacy | 5.51 | 1.169 | 0.920 |
| Respect for the patient and the parents | 5.70 | 0.748 | 0.918 |
| Paediatricians were empathetic | 5.70 | 0.878 | 0.918 |
| Nurses were empathetic | 5.63 | 0.912 | 0.919 |
| Consequences of treatment | 5.60 | 0.977 | 0.918 |
| Clear information about tests | 5.57 | 0.897 | 0.918 |
| Effects of drugs | 4.59 | 1.817 | 0.922 |
| Doctors and nurses worked closely together | 5.51 | 0.921 | 0.917 |
| Pain prevention and management | 5.48 | 1.084 | 0.920 |
| Active participation in decision-making | 4.95 | 1.553 | 0.921 |
| Could stay close to the child | 4.97 | 1.553 | 0.920 |
| Could stay close to child during invasive procedures | 5.20 | 1.614 | 0.923 |
| PICU cleanliness | 5.86 | 0.579 | 0.920 |
| Unit easily reached by phone | 3.15 | 2.814 | 0.939 |
| Low background noise | 4.87 | 1.279 | 0.923 |
| Enough space around child's bed | 5.35 | 1.152 | 0.921 |
| Team worked efficiently | 5.67 | 0.689 | 0.919 |
| Staff cared about the experience of parents | 5.02 | 1.461 | 0.918 |
| Discussed care daily with paediatricians | 5.60 | 0.926 | 0.919 |
| Discussed care daily with nurses | 5.54 | 1.000 | 0.919 |
| Paediatricians showed concern for the comfort of the child | 5.77 | 0.654 | 0.919 |
| Nurses showed concern for the comfort of the child | 5.70 | 0.761 | 0.919 |
| Identification of paediatricians in charge | 5.25 | 1.371 | 0.920 |
| Identification of nurses in charge | 5.20 | 1.396 | 0.921 |
| Confidence in paediatricians | 5.76 | 0.673 | 0.919 |
| Confidence in nurses | 5.62 | 0.892 | 0.920 |
| Information provided at discharge by paediatricians | 5.66 | 0.795 | 0.918 |
| Information provided at discharge by nurses | 5.55 | 0.961 | 0.919 |
The reliability of the domains of questionnaire, estimated by means of the Cronbach α, was fairly homogeneous, with values ranging between 0.72 and 0.89 except for the organisation domain, with a value of 0.56. The highest value, of 0.89, corresponded to the care and treatment domain. The values for the other domains were: parental participation, 0.72; information, 0.8; and professional attitude, 0.83. The Cronbach α for the overall questionnaire, based on standardised items, was 0.95, which is evidence of a high internal consistency.
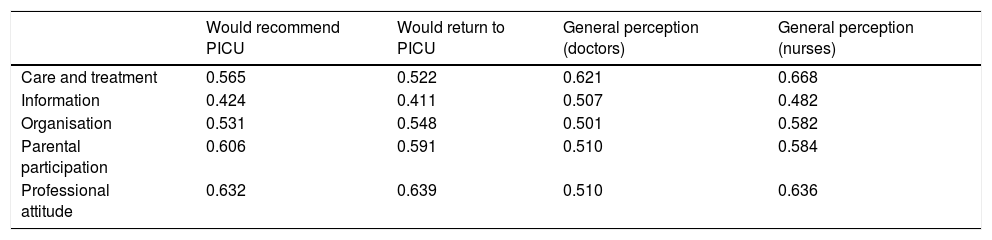
The internal validity of the questionnaire was assessed by calculating the correlation between the answers for the 5 domains and the 4 overall satisfaction questions, which was acceptable (Table 3).
Correlations between the different domains and the overall satisfaction items.
| Would recommend PICU | Would return to PICU | General perception (doctors) | General perception (nurses) | |
|---|---|---|---|---|
| Care and treatment | 0.565 | 0.522 | 0.621 | 0.668 |
| Information | 0.424 | 0.411 | 0.507 | 0.482 |
| Organisation | 0.531 | 0.548 | 0.501 | 0.582 |
| Parental participation | 0.606 | 0.591 | 0.510 | 0.584 |
| Professional attitude | 0.632 | 0.639 | 0.510 | 0.636 |
Significant correlation (p<.05).
The mean scores for the items “I would recommend this PICU to others” and “I would return to this PICU if I needed to” were 5.76 (SD, 0.54) and 5.69 (SD, 0.6), respectively. The scores reflecting the overall satisfaction with the physicians and nurses, with 1 being poor and 10 being excellent, were 9.43 (SD, 0.98) and 9.26 (SD, 1.2), respectively.
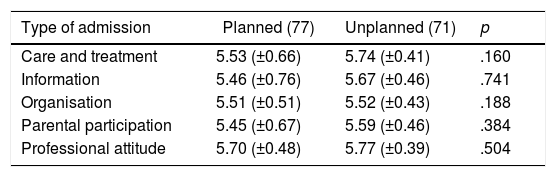
We did not find statistically significant differences in the scores of any of the domains based on whether admission was planned or urgent, the patient surgical or medical, or the patient needed or did not need mechanical ventilation (Table 4).
Comparative analysis of each domain by key characteristics: type of admission (planned/urgent; surgical/medical) and use of mechanical ventilation (yes/no).
| Type of admission | Planned (77) | Unplanned (71) | p |
|---|---|---|---|
| Care and treatment | 5.53 (±0.66) | 5.74 (±0.41) | .160 |
| Information | 5.46 (±0.76) | 5.67 (±0.46) | .741 |
| Organisation | 5.51 (±0.51) | 5.52 (±0.43) | .188 |
| Parental participation | 5.45 (±0.67) | 5.59 (±0.46) | .384 |
| Professional attitude | 5.70 (±0.48) | 5.77 (±0.39) | .504 |
| Type of patient | Post-surgical (77) | Not post-surgical (71) | p |
|---|---|---|---|
| Care and treatment | 5.54 (0.67) | 5.73 (0.41) | .246 |
| Information | 5.48 (0.74) | 5.67 (0.50) | .217 |
| Organisation | 5.46 (0.51) | 5.59 (0.43) | .151 |
| Parental participation | 5.45 (0.67) | 5.59 (0.45) | .475 |
| Professional attitude | 5.70 (0.49) | 5.78 (0.38) | .720 |
| Use of mechanical ventilation | Yes (77) | No (71) | p |
|---|---|---|---|
| Care and treatment | 5.71 (0.49) | 5.56 (0.63) | .197 |
| Information | 5.64 (0.511) | 5.50 (0.74) | .437 |
| Organisation | 5.59 (0.46) | 5.46 (0.49) | .056 |
| Parental participation | 5.61 (0.49) | 5.43 (0.69) | .280 |
| Professional attitude | 5.78 (0.40) | 5.69 (0.48) | .232 |
At present, measures of patient and family satisfaction are considered quality indicators in PICU performance.2,12
Until now, no validated questionnaires in Spanish have been published that assess the satisfaction of parents of children hospitalised in PICUs in Spain. The aim of our study was to translate the English version of the EMPATHIC-30 questionnaire to be used as a tool for assessment of quality of care as perceived by parents.
We chose this questionnaire because it has already been validated and used in several European countries (validated translations of the EMPATHIC-65 version exist in Dutch, English,10 French13 and Italian,14 among other languages). They derive from the original EMPATHIC-65 questionnaire developed by the research team led by Latour.10 The shortened EMPATHIC-30 version allows for quicker completion while retaining the reliability and internal consistency of the original. We translated the questionnaire following the guidelines for translation and validation proposed by the ISPOR,11 which, as explained in the methods section, involved 10 steps. The pilot test was conducted on 10 parents or legal guardians of patients staying in the PICU. All the surveyed parents reported that they found the questionnaire easy to understand, not too long, and appropriate for its intended use. We estimated that the time required for its completion is of approximately 10min. There is evidence in the literature that the length of the questionnaire is not relevant in assessing satisfaction,15 but we considered that as long as reliability was not compromised, shortening the questionnaire had the advantage of making it easier for families to complete it.9
In our study, in contrast with the evaluation of the original questionnaire, where the latter was sent by mail to the parents 2–3 weeks after discharge from the PICU, we gave parents a copy of the questionnaire at the time of discharge. Once completed, parents could drop them in the boxes arranged for that purpose in the PICU and the inpatient wards. We expected that this would increase the response rate. We do not know the exact number of questionnaires that were given out or of responses received, but we estimate that more than 90% of the distributed questionnaires were completed.
Sixty-four percent of questionnaires were completed by mothers and 34% by fathers. We found no differences in the responses between planned and urgent admissions, medical and surgical patients, or patients that received mechanical ventilation and patients that did not. The Italian questionnaire study14 found a higher level of satisfaction in patients whose admission had been planned. The authors believed this could have been due to parents and patients being better informed about admission and hospitalisation procedures.16
Most parents in our study were of Spanish origin, so there was no cultural heterogeneity that may have altered the perception of questionnaire items. In the study of the original questionnaire in Dutch there was significant cultural diversity, with a high proportion of immigrants among the participants. This could pose greater challenges in areas in Spain with larger immigrant populations.
In our study, the mean score was less than 5 for five of the thirty items. The items with the lowest mean scores corresponded to the information regarding treatment (4.59), shared decision-making (4.95), encouragement to stay close to the child (4.97), ease of reaching the PICU by phone (3.15) and the background noise in the unit (4.87). The policy of allowing access to the unit 24h a day was introduced in 2013 and had only been in place for 1 year when the study was conducted.
Scores of less than 5 in these items may have been due to the reasons that follow.
On one hand, health care professionals are not used to having families participate in decision-making. On the other, the initial response of health professionals to allowing the presence of parents 24h a day is usually negative. There is evidence that ICU staff experience distress in the initial stages of unlimited, open access to the unit, as is usually the case with any significant organisational change. However, once the change has been made, most of the staff perceive it in a positive light.17
Another factor at play is the frequent use by physicians when explaining treatments of medical terminology that is not adapted to the comprehension level of parents.
When it comes to the background noise, in addition to the loud voices frequently used by the health care staff, the architecture of the unit played a role in our study, as the ceilings are low and amplify sound.
The item regarding the “phone” was a different matter: the score in this item was associated with parents not needing to use this medium to obtain information about their children. Since parents could stay in the unit 24h a day and were able to use their own phones, they did not need to resort to using the phone line of the unit. Of a total of 132 participants that gave an answer for this item, 52 (34.7%) selected the “not applicable” option, 57 (38%) responded they fully agreed, and 15 (10%) responded that they agreed, so we may conclude that those parents that used this medium to obtain information found it a useful means to be apprised of the condition of their children. Nevertheless, we believe that this was a necessary item to assess parental ease of mind in knowing that they can call at any time to ask about the condition of their children.
The results of reliability tests were in the same range as those of the original studies, with internal consistency values greater than 0.7 except in the organisation domain, where we obtained a Cronbach α of 0.56. This result may be due this domain including the item regarding phone access, which 12% of respondents did not answer and another 35% considered “not applicable,” possibly affecting the overall α value.
The internal consistency of the questionnaire was confirmed by the acceptable correlation of the general satisfaction items and the 5 domains of the questionnaire.
Chief among the limitations of our study is that it was conducted in a single Spanish PICU and in a specific autonomous community, so its results may not be representative of all PICUs in Spain. The next step in the process would be to ask other PICUs to participate in a broader assessment of this questionnaire.
A second important limitation is that the sample under study consisted mainly of Spanish nationals, with a small proportion of immigrants. Last of all, we did not compare these initial results with the results obtained from a second cohort at a different time, as recommended by other authors.18 In the original study by Latour et al., the questionnaire was evaluated in 2 cohorts at different times, which demonstrated the reliability of the questionnaire.
In conclusion, we believe that the translation and cultural adaptation of the EMPHATIC-30 questionnaire for the Spanish population provides a valid and reliable tool to assess the satisfaction of parents with PICU services. This tool can help professionals identify areas for quality improvement in family-centred care. It can also serve as a benchmarking tool19,20 in Spanish PICUs.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank our hospitalised patients and their families.
| Item | 1 | 2 | 3 | 4 | 5 | 6 | Not applicable | No answer |
|---|---|---|---|---|---|---|---|---|
| 1 | 2 (1.3) | 1 (0.7) | 7 (4.7) | 19 (12.7) | 118 (78.7) | 3 (2) | ||
| 2 | 2 (1.3) | 1 (0.7) | 3 (2) | 4 (2.7) | 19 (12.7) | 117 (78) | 1 (0.7) | 3 (2) |
| 3 | 1 (0.7) | 1 (0.7) | 4 (2.7) | 7 (4.7) | 26 (17.3) | 111 (74) | ||
| 4 | 3 (2) | 4 (2.7) | 8 (5.3) | 22 (14.7) | 24 (16) | 71 (47) | 14 (9) | 4 (2.7) |
| 5 | 1 (0.7) | 1 (0.7) | 5 (3) | 6 (4) | 27 (18) | 108 (72) | 2 (1.3) | |
| 6 | 1 (0.7) | 1 (0.7) | 2 (1.3) | 3 (2) | 37 (25) | 102 (68) | 2 (1.3) | 2 (1.3) |
| 7 | 3 (2) | 2 (1.3) | 5 (3.3) | 17 (11.3) | 32 (21) | 81 (54) | 5 (3.3) | 5 (3.3) |
| 8 | 2 (1.3) | 2 (1.3) | 11 (7) | 12 (8) | 24 (16) | 90 (60) | 5 (3.3) | 4 (2.7) |
| 9 | 2 (1.3) | 3 (2) | 7 (4.7) | 21 (14) | 103 (68.7) | 11 (7.3) | 3 (2) | |
| 10 | 1 (0.7) | 1 (0.7) | 1 (0.7) | 1 (0.7) | 26 (17) | 118 (78.8) | 2 (1.3) | |
| 11 | 1 (0.7) | 1 (0.7) | 4 (2.7) | 27 (18) | 108 (72) | 4 (2.7) | 5 (3.3) | |
| 12 | 1 (0.7) | 1 (0.7) | 10 (6.7) | 138 (92) | ||||
| 13 | 2 (1.3) | 1 (0.7) | 5 (3.3) | 15 (10) | 57 (38) | 52 (35) | 18 (12) | |
| 14 | 3 (2) | 6 (4) | 10 (7) | 21 (14) | 37 (25) | 72 (48) | 1 (0.7) | |
| 15 | 3 (2) | 3 (2) | 7 (4.7) | 8 (5.3) | 29 (19) | 100 (67) | ||
| 16 | 1 (0.7) | 1 (0.7) | 4 (2.7) | 30 (20) | 113 (75) | 1 (0.7) | ||
| 17 | 1 (0.7) | 3 (2) | 2 (1.3) | 22 (15) | 121 (81) | 1 (0.7) | ||
| 18 | 3 (2) | 2 (1.3) | 6 (4) | 13 (8.7) | 36 (24) | 80 (53.3) | 5 (3.3) | 5 (3.3) |
| 19 | 1 (0.7) | 2 (1.3) | 7 (4.7) | 23 (15.3) | 112 (75) | 2 (1.3) | 3 (2) | |
| 20 | 1 (0.7) | 1 (0.7) | 1 (0.7) | 8 (5.3) | 23 (15.3) | 107 (71.3) | 2 (2.3) | 7 (4.7) |
| 21 | 2 (1.3) | 5 (3.3) | 18 (12) | 120 (80) | 5 (3.3) | |||
| 22 | 1 (0.7) | 2 (1.3) | 5 (3.3) | 18 (12) | 118 (79) | 6 (4) | ||
| 23 | 3 (2) | 2 (1.3) | 4 (2.7) | 12 (8) | 21 (14) | 100 (67) | 4 (2.7) | 4 (2.7) |
| 24 | 3 (2) | 1 (0.7) | 5 (3.3) | 14 (9.3) | 21 (14) | 96 (64) | 4 (2.7) | 6 (4) |
| 25 | 1 (0.7) | 1 (0.7) | 4 (2.7) | 17 (11) | 124 (83) | 3 (2) | ||
| 26 | 2 (1.3) | 1 (0.7) | 7 (4.7) | 21 (14) | 114 (76) | 5 (3.3) | ||
| 27 | 2 (1.3) | 1 (0.7) | 5 (3.3) | 15 (10) | 122 (81) | 1 (0.7) | 4 (2.7) | |
| 28 | 1 (0.7) | 1 (0.7) | 1 (0.7) | 6 (4) | 21 (14) | 114 (76) | 1 (0.7) | 5 (3.3) |
| 29 | 1 (0.7) | 2 (1.3) | 9 (6) | 15 (10) | 115 (77) | 8 (5.3) | ||
| 30 | 1 (0.7) | 1 (0.7) | 7 (4.7) | 24 (16) | 100 (66.7) | 2 (1.3) | 15 (10) |
Answer distribution. Absolute frequencies and percentages: n (%).
Please cite this article as: Pilar Orive FJ, Basabe Lozano J, López Zuñiga A, López Fernández YM, Escudero Argaluza J, Latour JM. Traducción y validación al español del cuestionario EMPATHIC-30 para medir la satisfacción de los padres en cuidados intensivos. An Pediatr (Barc).2018;89:50–57.
☆ Previous presentations: This study was presented as an oral communication under the title Traducción, validación al español del cuestionario EMPHATIC-30 para medir la satisfacción de los padres en la unidad de cuidados intensivos de pediatría at the XXXII Congress of the Sociedad de Cuidados Intensivos Pediátricos; May 4-6, 2017; Granada, Spain.