Research is the cornerstone of medical progress. Paediatric research has its own nuances and represents an additional challenge due to the intrinsic characteristics of the paediatric population compared with adults. Despite the tremendous importance of childhood health and its impact during adulthood, society is still not convinced about the importance of conducting research in paediatrics. This also applies to paediatricians themselves, who think about research as a discipline that does not directly involve them.
The Spanish Academy of Paediatrics has developed a specific research platform- INVEST-AEP- to try to help and answer the challenges associated with paediatric research in the society. This article reflects the current status of paediatric research in Spain, and the goals achieved over the last few years due to the effort of paediatric researchers. In addition, a deeper analysis is provided as regards: (a) the barriers that represent a hurdle for the development of broad and competitive paediatric research in our day to day work; (b) the limited incentives and specific pre- and post-doctoral training; (c) the high clinical burden for paediatricians or; (d) the lack of specific infrastructure and dedicated funding for paediatrics. The mission, vision and values of INVEST-AEP are to develop an accessible roadmap for the development and implementation of paediatric research in Spain for the next few years.
La investigación clínica es la piedra angular para el desarrollo de la Medicina, y, en el ámbito de la Pediatría, supone un reto adicional debido a las peculiaridades que diferencian a los niños de los adultos. A pesar del enorme impacto de la salud infantil en el resto de la vida, nuestra sociedad aún no está suficientemente concienciada sobre la importancia de la investigación pediátrica, que, en general, se encuentra también muy alejada del día a día de quienes nos dedicamos a esta profesión.
Desde la Asociación Española de Pediatría (AEP) se ha creado una plataforma específica de investigación —INVEST-AEP— para dar respuesta específica a los retos de la investigación en el seno de nuestra sociedad. En este artículo se retrata el escenario actual de la investigación pediátrica en España y se objetivan las metas alcanzadas en los últimos años, gracias al esfuerzo de los pediatras investigadores. Además, se realiza un análisis en profundidad sobre las barreras cotidianas que dificultan el desarrollo amplio y competitivo de la investigación pediátrica, como la falta de incentivación y ausencia de formación específica de pre y posgrado, la elevada carga asistencial o la falta de infraestructuras y financiación específicas. Definimos la misión, visión y valores de INVEST-AEP para tratar de diseñar una «hoja de ruta» para la investigación pediátrica española de los próximos años.
No paediatrician would hesitate if they were asked about the need for research in our specialty. We all know that children have particular physiological characteristics: they are not even a homogeneous group of patients, as their diseases, the way in which they manifest and their severity vary between age groups. We are all aware in our daily practice of the differences in pharmacokinetics and pharmacodynamics compared to adults. We all know that this hinders the generalisation and practical application of the results of studies conducted in adults to paediatric patients of different ages—from newborns to adolescents. As paediatricians, we cannot help but know how few drugs are authorised for use in children, and we know that it is in childhood that the identification of risk factors for health can have the most impact on subsequent stages of life, and that this is the period when preventive interventions may be most beneficial in the short and the long term. Yet, few of us place research in paediatrics among our priorities. Why?
We ought to reflect and ask ourselves some questions related to research in paediatrics: Do we convey to our youth the importance of being a leader in science, and not a mere observer? Do we teach students in medical school or residents in paediatrics how to start and develop a research project? Does the culture in our workplace promote research? Do we set aside time during the workday to carry out this work? In this article, and from the Platform for Research in Paediatrics of the Asociación Española de Pediatría (INVEST – AEP), we attempt to address these questions and to encourage a deep reflection on the everyday obstacles that hinder research in paediatrics.
Research in paediatrics: what is the status quo?What better proof is there of the need to conduct research in paediatrics than the limited number of drugs approved for use in children, which affects our practice on a daily basis? In Europe, only 30% of drugs in the market are authorised for use in the paediatric population, and fewer than 50% of drugs authorised for use in this age group have been tested in paediatric clinical trials, as the European Union has officially acknowledged.1 Therefore, children frequently receive drugs that have not been validated for their age and whose assumed benefits are extrapolated from studies conducted in adults.2 The use of drugs that have not been authorised for paediatric use is not free of risk, as they can have unexpected side effects due to either ineffectiveness or toxicity. If we consider the summary of product characteristics as a standard of good clinical practice, the use of drugs that have not been authorised in children can have ethical and legal repercussions associated with poor clinical practice. However, if we were to withhold drugs authorised for adults, we would be denying children a potentially beneficial intervention. From this perspective, research in paediatrics should not only be ethically feasible but also essential to good clinical practice.
While the overall paediatric population should be a priority in scientific research, the need for research is even more urgent in specific groups of patients, such as newborns, critically ill children or patients with rare or infrequent diseases. In the late 1990s, several studies brought to light that 64.6% of prescriptions made in neonatal units were for off-label use or for drugs not authorised in this population.5 Fifteen years later, studies show nearly interchangeable figures, which is all the more alarming when we focus on the group of very preterm newborns, in whom nearly every prescription is off-label and for whom data on pharmacokinetics and pharmacodynamics are all but non-existent.6,7 Children with rare diseases are another neglected group of patients, as confirmed by the European Medicines Agency (EMA) in its latest report. In this group, it is frequently not even possible to extrapolate data from adult studies, as these patients often suffer from disorders that characteristically manifest in childhood or adolescence, and therefore any advances in their understanding depend solely on us. In any case, there is still much to learn even in the most frequent disorders, such as bronchiolitis, one of the most prevalent diseases of childhood for which we have yet to find effective preventive or therapeutic interventions, mainly because the underlying pathophysiology is not well understood.
The European Commission recognised this problem, and in December 2006 introduced Regulation No. 1901/2006 on medicinal products for paediatric use to try to alleviate this situation, introducing a system for the development of paediatric investigation plans (PIPs) to be evaluated by the Paediatric Committee of the EMA (PDCO). A decade later, research on paediatric drugs has increased substantially, although the number of trials including children has only increased by 50%, which means there is still room for improvement, especially in certain therapeutic areas. This situation, and following the report published by the Commission in October 2017,3 has led to the development of an action plan by the European Commission, the EMA and its PDCO that is currently being implemented with substantial collaboration from different organisations. Thus, the European Commission is engaged in the establishment of a pan-European paediatric clinical trial network known as Connect-4-Children (https://conect4children.org) and promoting initiatives through the Horizon 2020 programme, such as the European Paediatric Translational Research Infrastructure (EPTRI), which aims at establishing the foundations for a new scientific infrastructure.4
The boom of paediatric research networks in SpainIn recent decades, the number of research networks in every field of paediatrics has multiplied, facilitating the exchange of knowledge and resources between researchers who are physically distant, and launching Spanish research into the international scene.
Collaboration through networks is crucial in paediatrics, as it helps overcome the logistic, methodological and ethical barriers that affect research in children due to the low prevalence of some diseases, the lack of resources and the geographical dispersion of our patients. Networks promote the exchange of resources and knowledge between researchers in different fields and the standardisation of methodologies, and they shorten the time needed to obtain statistically significant results. Furthermore, they increase the chances of receiving funding through competitive grants and provide opportunities for career advancement, as they lead to contact with other specialists and participation in projects that are difficult to get involved in outside of these structures.8–11
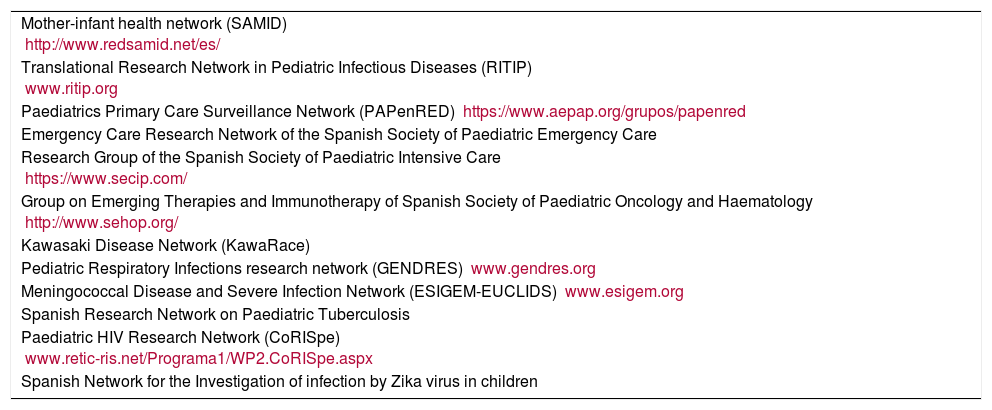
In Spain, collaboration through networks has considerably enriched paediatric research, with interesting examples in areas as diverse as mother and infant health (Red de Salud Maternoinfantil [SAMID], http://www.redsamid.net/es/), the only paediatric network funded by the Instituto de Salud Carlos III, Translational research network in pediatric infectious diseases (Red de Investigación Traslacional en Infectología Pediátrica [RITIP], www.ritip.org) or the creation of a paediatric primary care surveillance network (Red de Vigilancia en Pediatría de Atención Primaria [PAPenRED], https://www.aepap.org/grupos/papenred). Technological advances and the widespread availability of data collection platforms have allowed the proliferation of thematic networks focused on specific diseases in every paediatrics specialty (Table 1).
Examples of paediatric research networks in Spain.
| Mother-infant health network (SAMID) http://www.redsamid.net/es/ |
| Translational Research Network in Pediatric Infectious Diseases (RITIP) www.ritip.org |
| Paediatrics Primary Care Surveillance Network (PAPenRED) https://www.aepap.org/grupos/papenred |
| Emergency Care Research Network of the Spanish Society of Paediatric Emergency Care |
| Research Group of the Spanish Society of Paediatric Intensive Care https://www.secip.com/ |
| Group on Emerging Therapies and Immunotherapy of Spanish Society of Paediatric Oncology and Haematology http://www.sehop.org/ |
| Kawasaki Disease Network (KawaRace) |
| Pediatric Respiratory Infections research network (GENDRES) www.gendres.org |
| Meningococcal Disease and Severe Infection Network (ESIGEM-EUCLIDS) www.esigem.org |
| Spanish Research Network on Paediatric Tuberculosis |
| Paediatric HIV Research Network (CoRISpe) www.retic-ris.net/Programa1/WP2.CoRISpe.aspx |
| Spanish Network for the Investigation of infection by Zika virus in children |
At the same time, these nationwide networks have leaned on solid infrastructures to create biobanks focused on different diseases, such as the HIV Biobank of the Hospital Gregorio Marañón (HGM) or the Biorepository of samples of the network for the study of paediatric tuberculosis (pTBred), both of which are housed in the same physical location, the Biobanco VIH-HGM. Biobanks expand the boundaries of paediatric research, as they guarantee the quality of samples to perform, for instance, genomic studies about individual risk, or studies aimed at identifying new molecular markers for diagnosis or assessment of therapy response.
When it comes to clinical trials, a Spanish network for paediatric clinical trials was created in 2017 (Red Española de Ensayos Clínicos Pediátricos [RECLIP], www.reclip.org); it is coordinated form the Hospital Clínico Universitario in Santiago de Compostela and includes the main units involved in clinical trials, facilitating the development of a collaborative infrastructure for the safe and effective performance of paediatric trials. This has made it possible for Spain to join the Conect-4-Children network (www.conect4children.org), which has recently received funding through a grant from the Innovative Medicines Initiative (IMI) 2, and whose aim is to promote paediatric clinical trials in Europe.
Spanish research in paediatrics has also reached continental scope through participation in the European Reference Networks (ERNs),12 which help share and disseminate the experience in rare diseases between different countries. To date, 24 ERNs have been created, including the “TRANSplantChild”, www.transplantchild.eu/en/, a network led by the Hospital Universitario La Paz dedicated to paediatric solid organ and haematopoietic stem cell transplantation from a cross-sectional, multidisciplinary and holistic perspective, and focused on clinical issues that are common to different paediatric transplantation procedures.
On the other hand, the Spanish SAMID, RECLIP and RITIP networks have recently been accredited as networks of excellence by the European Network of Paediatric Research of the European Medicines Agency (EnprEMA), acknowledging their activity in research and education.
Despite this significant boost in research, the volume of research projects and initiatives and of resources obtained from national and international competitive grants in the sector of Spanish paediatrics is not yet commensurate with the position and size of our society.
Awareness in research: from education to institutions, in collaboration with the community.
One of the main barriers to the fulfilment of the research potential in the collective of paediatricians in our country is the lack of a culture of biomedical research in Spain. The promotion of research requires providing adequate training and incentives to future specialists from the time they start their undergraduate education in schools of medicine and through their specialty residency trainings (the MIR programme in Spain). Future paediatricians must come to understand that research and clinical practice are intimately related and that improvement in patient care is tied to the performance of research studies. With the Bologna Process, the new educational approach is finally prioritising the development of practical skills in schools of medicine. However, training in scientific methodology (literature searches, critical reading, statistical analysis, scientific writing and communication) is not integrated transversally in each subject. Biomedical research should likewise be considered an essential component of the curriculum of residencies in paediatrics, parallel to the development of clinical skills. The MIR residency curricula should include, and teaching hospitals offer, the opportunities and resources that physicians-in-training require to be involved in research projects, allocating time specifically to this activity. Last of all, after physicians have completed their residency, professional involvement in research should be encouraged and recognised, establishing the necessary structure to allow research to be pursued in parallel to clinical practice.
Training health professionals in research and making them aware of its importance are both key to improving our knowledge and thus the health of our patients, but without the involvement of institutions, excellence in research will remain an unattainable dream. Institutions are responsible for structuring the strategies needed to harmonise care delivery, research and education, and they must promote pathways for career development that emphasise research skills and experience in order to attract and hold talent in this field. However, there are still innumerable professional barriers, which are hard albeit not impossible to overcome, such as the lack of time specifically allocated to research when there is no funding, the overwhelming caseloads, the near absent interaction with other fields, the absence of the necessary infrastructure for conducting research in hospitals, the excessive bureaucracy or the lack of funding. This is further compounded by the lack of incentives for paediatricians that conduct research as part of their regular work, and the fact that this activity is not taken into account in the ranking schemes applied to professional promotion.
The participation of the community in studies and clinical trials through the collaboration with patient associations would be highly beneficial. Paediatric researchers should reach out to children, parents and their families to encourage them to get involved and demand further and better research in paediatrics, as well as their participation in undergoing clinical trials, recruitment efforts, etc. These views are shared by different organisations, including the European Foundation for the Care of Newborn Infants (EFCNI), the European Patients’ Academy on Therapeutic Innovation (EUPATI) and the EnprEMA.
Another essential element for research in paediatrics is the development of research partnerships with the private sector. The involvement of industry has allowed the establishment of key synergies that support most of the cutting-edge research in Spain due to the cuts to the public R+D budget. Still, the continued and organised provision of human and material resources for research in health should be the responsibility of the public authorities and a priority in the general budget of the state. More specifically, governmental organisations that are involved in research ought to promote, prioritise and fund research on subjects related to paediatrics when it comes to awarding future competitive grants.
All of these barriers evince the need for a coordinated effort on the part of institutions and scientific societies to develop improvement strategies aimed at achieving excellence in translational research in paediatrics, because the talent required is out there. We need to find the way to translate the findings of basic research into improvements in patient care in the field of paediatrics. And it is not possible to conceive of a future society in which research is not part of the professional activity of physicians.
Ethical considerations in paediatric researchChildren constitute a particularly vulnerable population, and therefore paediatric researchers need to know the regulations that govern research in humans and the special implications of research in paediatrics. Any research activity that involves children must balance out the need to investigate with the duty to protect the wellbeing of our patients and strict adherence to the Rights of the Child,13 guaranteeing their protection as individuals, since minors are not legally capable of providing consent and may have limited understanding and decision-making abilities, thus depending on adults for protection. Therefore, informed consent must always be obtained from the parents or legal guardians, in addition to consent from mature minors aged more than 12 years. Researchers must be aware that any study they undertake must have been approved by an accredited ethics committee, which needs to consider how to minimise risk and whether the benefit-cost ratio is reasonable.14
There are several laws that regulate the participation of minors in clinical trials to protect them from risk and to safeguard their autonomy. Royal Decree 1090/2015 of December 4 2015 (B.O.E 24-12-2015) on the regulation of clinical trials of medicines provides a legal framework for the performance of clinical trials in minors in article 5. For these reasons, ethics committees that oversee research involving medicines should include members with expertise in paediatrics or obtain guidance on the clinical, ethical and psychosocial issues that are relevant in the field of paediatrics.
INVEST-AEP: the answer of the Spanish Pediatric Association to the current needs in paediatric researchIn this context, the Asociación Española de Pediatría (Spanish Association of Paediatrics, AEP) has established a platform, the INVEST-AEP, with the objective and mission of promoting research in paediatrics mainly carried out by paediatricians, both in hospital and primary care settings, through incentives, training, active promotion, facilitation, guidance, recognition and the provision of the resources that our paediatricians need to conduct competitive and high-quality research. This investment expresses a resolute stance from the AEP, whose vision is that research is one of the pillars of the daily health care practice of paediatricians, independently of their specialty, and that paediatricians must lead and get involved in ideas, projects and multidisciplinary networks in Spain and at the international level. In this way, through this platform, the AEP aspires to achieve excellence in paediatric research, always in the context of ethics and quality. We are aware of the enormous responsibility we have as drivers of change in the paediatric community and in promoting translational research for application to everyday clinical practice.
Some of the priority strategic plans contemplated by the INVEST-AEP is contributing to the training in research of paediatricians, and therefore, we consider it a priority to convey to the competent authorities in the Ministry of Education, through the Commission on specialties and under the leadership of the Board of Directors of the AEP, the need to include specific training on research both at the undergraduate and the post-graduate medical education. We need to create a critical mass of researchers capable of carrying out high-quality projects and joining already existing groups. Our aim is to encourage sponsorship by having renowned research teams in Spain working domestically and in collaboration with groups in other countries, and to establish a pool of health facilities willing to host and oversee the work of young researchers. It is just as important to create awareness in institutions regarding funding, both public and private, that paediatric research deserves a distinct and independent treatment in relation to research in adults, with at least equal consideration when it comes to the allocation of resources. On its part, the AEP must provide resources to promote research, among others through calls for competitive grants. It is the wish of this platform that young researchers benefitting from these grants, in particular those devoted to education, join the INVEST-AEP to eventually contribute to train the next generation of young paediatricians. Raising social awareness and involving children, parents and their families in this platform will be one of our priorities.
Conflict of interestAsuncion Mejias has received grant funding (to institution) from Janssen and honoraria for CME lectures from Abbvie.
Please cite this article as: Calvo C, Sainz, Codoñer-Franch P, Santiago B, García-García ML, García Vera C, et al. La investigación en Pediatría en España: retos y prioridades. Plataforma INVEST-AEP. An Pediatr (Barc). 2018;89:314.